Hospital-at-home programs have expanded rapidly across the U.S., but most patients have no idea this option exists when facing admission.
When my husband George was cycling through hospital stays every month for his end-stage renal disease and cancer in 2018, nobody told us there might be another way. We assumed the hospital was our only option. Month after month, we dealt with the ER waits, the uncomfortable chairs, the sleepless nights, and the parade of specialists who never seemed to talk to each other.
Things have changed since then. Hospital-at-home care has gone from experimental to mainstream. Medicare now covers it permanently. Your insurance probably covers it too.
But you have to know to ask for it.
Let’s break down everything you need to know about hospital-at-home versus traditional hospitalization, including:
- a comparison of clinical outcomes
- the hidden costs nobody talks about
- how to decide which option makes sense for your situation
Contents
- What Is Hospital at Home Care?
- How Traditional Hospital Care Works
- Clinical Outcomes: Which Delivers Better Results?
- The Hidden Costs Nobody Tells You About
- What the Caregiver Experience Actually Looks Like
- How to Know if Hospital at Home is Right for Your Situation
- How to Access Hospital-at-Home Programs
- Questions to Ask Before You Decide
- Making the Right Choice for Your Family
What Is Hospital at Home Care?

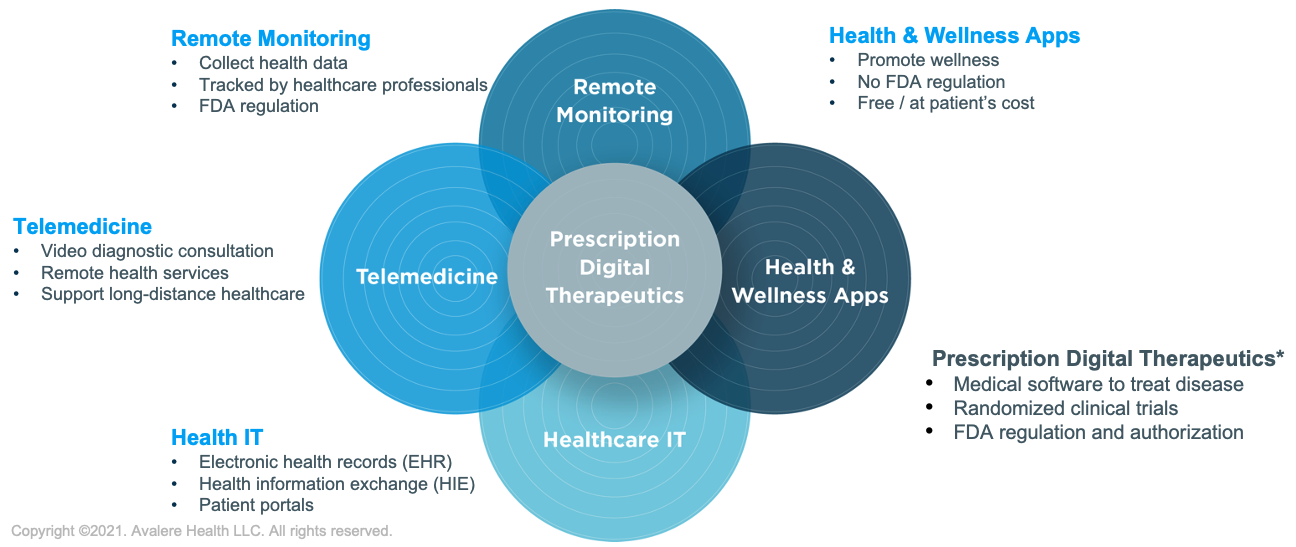
Hospital-at-home means exactly what it sounds like: you receive acute-level medical care in your own home instead of in a hospital facility. This isn’t the same as regular home healthcare or skilled nursing. We’re talking about the same intensity of care you’d get if you were admitted to a hospital bed.
What conditions qualify for hospital-at-home care?
You can receive hospital-at-home care for conditions like pneumonia, COPD flare-ups, heart failure, serious infections, and certain post-surgical recoveries. A 2023 study in the Annals of Internal Medicine found that hospital-at-home programs safely treated patients with cellulitis, urinary tract infections, and heart failure exacerbations.
The key word here is “acute.” You need to be sick enough to require hospitalization, but stable enough to be safely monitored at home.
What does hospital-level care actually include?

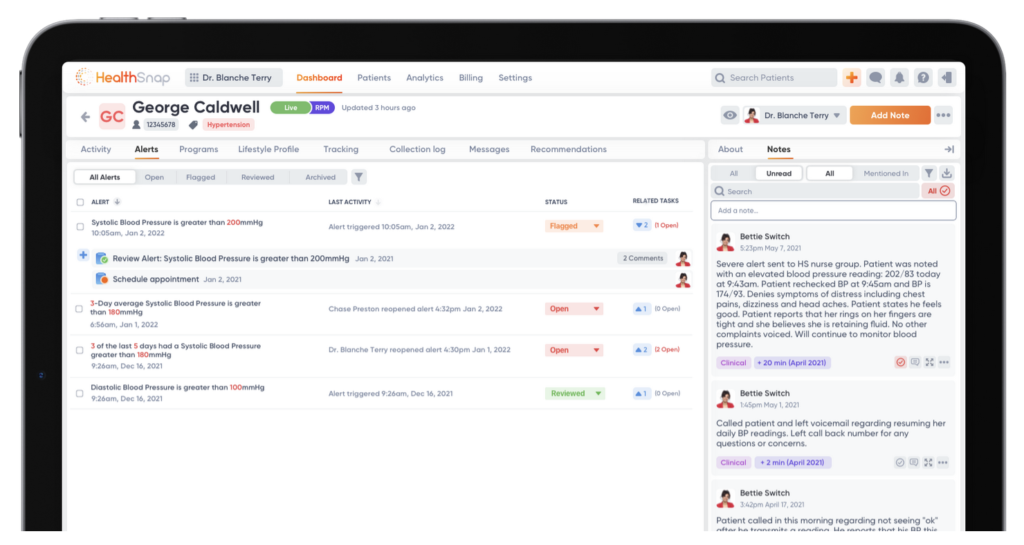
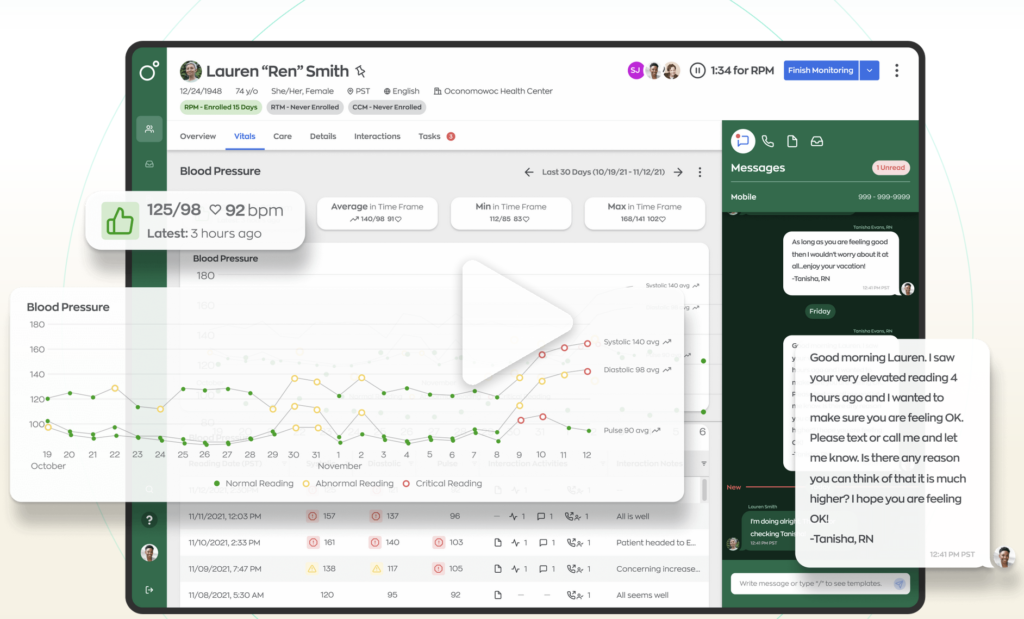
Your care team visits you at home daily, and sometimes twice a day. This includes physicians, nurses, physical therapists, and care coordinators. You’ll get IV medications if you need them. You’ll wear devices that monitor your vital signs and send data to your medical team in real-time. It’s like having a hospital room set up in your living room, but without the hospital smell and terrible food.
When George was using his Dexcom continuous glucose monitor, I got alerts on my phone whenever his blood sugar spiked or dropped dangerously low. That technology exists for heart rate, oxygen levels, blood pressure, and more. Your care team watches these numbers from their computers and can intervene before small problems become emergencies.
Who provides the care?
A dedicated hospital-at-home team manages your case. You’ll have a primary physician who oversees your treatment plan. Nurses visit to check on you, administer medications, and assess your condition. The big difference from traditional home health? These visits happen daily, and you have 24/7 access to your care team by phone or video.
The shift from experimental to mainstream happened fast. Before COVID-19, only a handful of health systems offered hospital-at-home programs. The pandemic forced rapid expansion, and in 2025, the Hospital Inpatient Services Modernization Act extended the CMS waiver to continue providing hospital-at-home care.
How Traditional Hospital Care Works

When you’re admitted to a traditional hospital, you check in through the emergency department or for a scheduled admission. A nurse takes your vitals, you change into a hospital gown, and you’re assigned to a room (if one’s available—sometimes you wait for hours).
The hospital routine
Nurses check your vitals every few hours, day and night. Yes, even at 3 a.m. Doctors round in the morning, usually between 7 and 10 AM. If you’re asleep when they come by, too bad. Meals arrive on a fixed schedule whether you’re hungry or not.
With George’s 10 different specialists, we never knew who would walk through the door or when. His nephrologist didn’t talk to his oncologist. His endocrinologist had no idea what his cardiologist prescribed. I became the central hub of information, keeping my own spreadsheet because the hospital’s electronic records didn’t seem to connect the dots.
Family involvement and visiting limitations

Even before COVID-19 restrictions, hospitals limited visiting hours. During the pandemic, many hospitals banned visitors entirely. In 2025, most facilities still have restrictions like limited hours, limited number of visitors, no children under 12.
If you want to be there when doctors round to ask questions, you’d better arrive early and stay all day.
Need to go home to shower or check on your kids? You might miss critical conversations about your loved one’s treatment plan.
The discharge process often feels rushed. A nurse reviews a stack of papers, hands you prescriptions, and sends you on your way. Studies show 20% of patients don’t understand their discharge instructions.
Clinical Outcomes: Which Delivers Better Results?
Does hospital-at-home actually work as well as traditional hospitalization?
Yes—and sometimes better.
Patient satisfaction scores
A 2024 meta-analysis in JAMA Network Open reviewed 25 studies comparing hospital-at-home care to traditional care. Patient satisfaction scores were consistently higher for hospital-at-home, with 87% of patients rating their experience as “excellent” compared to 62% for traditional hospitalization.
That’s not surprising. People sleep better when they’re in their own beds. They get to eat their own food, and see their family members whenever they want.
The medical care is just as good, but the experience is dramatically better.
Hospital readmission rates

Getting sent back to the hospital within 30 days of discharge is a sign something went wrong.
For traditional hospitalizations, the 30-day readmission rate hovers around 15% to 20% depending on the condition. Hospital-at-home programs report readmission rates of 8% to 12%.
That’s because closer monitoring catches problems earlier. Patients understand their care plan better because they’re not overwhelmed and sleep-deprived. The transition from acute care to regular life is smoother when you’re already home.
Infection risk and recovery time
Hospital-acquired infections affect 1 in 31 hospital patients on any given day, according to the CDC. At home, you’re not exposed to antibiotic-resistant bacteria floating around hospital wards. You’re not sharing air with other sick people.
Recovery happens faster when you’re comfortable and less stressed. A 2023 study found that elderly patients receiving hospital-at-home care regained their ability to perform daily activities 40% faster than those in traditional hospitals.
The mortality rates? Comparable. For appropriate patients, hospital-at-home is just as safe as traditional hospital care.
The Hidden Costs Nobody Tells You About
The hospital bill is just the beginning. Let’s talk about what you’ll actually pay and what costs don’t show up on an invoice.
Out-of-pocket expenses for traditional hospitalization
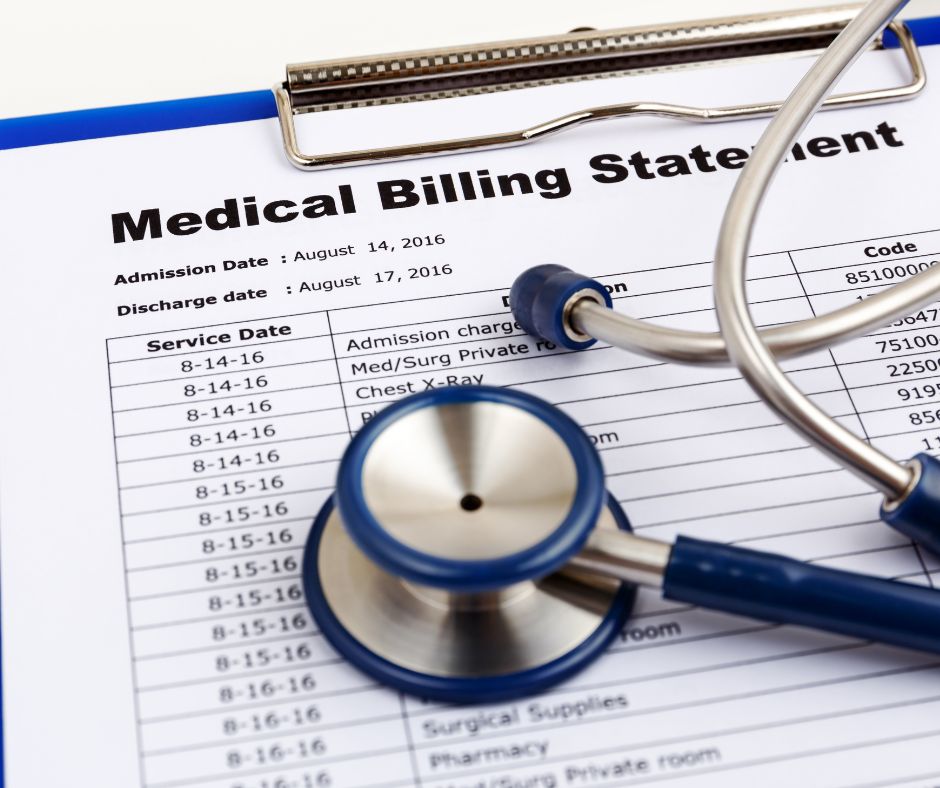
Even with good insurance, a three-day hospital stay can cost you $1,500 to $3,000 in co-pays and deductibles. That’s the baseline. Then come the surprise charges.
Facility fees can add hundreds of dollars:
- Labs processed by an out-of-network pathologist costs extra.
- The ambulance ride is often not fully covered.
- According to a 2019 report, 1 in 5 emergency hospital visits result in at least one surprise bill averaging $750.
And let’s not forget parking. $15 per day adds up when you’re visiting daily for weeks. Hospital cafeteria meals for family members is $10 to $15 each.
These “small” costs can easily hit $500 to $1,000 for a typical hospital stay.
Out-of-pocket expenses for hospital at home

Medicare covers hospital-at-home the same way it covers traditional hospitalization. You pay the standard hospital deductible and any applicable co-pays. Most private insurers follow Medicare’s lead, but coverage varies.
The surprise? Hospital-at-home often costs you less out-of-pocket because there’s no:
- parking fees
- expensive hospital cafeteria meals
- co-pays for separate facility charges
A 2021 analysis found that patients in hospital-at-home programs saved an average of $2,400 in out-of-pocket costs compared to traditional hospitalization.
You might need to buy a few things—maybe a shower chair or grab bars if you don’t have them. But the program provides equipment like IV poles and monitoring devices.
The invisible costs for caregivers
The economic impact on caregivers is often overlooked. I burned through my vacation days and sick leave taking George to appointments and managing his care, even while working remotely. Many caregivers do the same.
The financial burden is more than just lost wages. A 2023 AARP study found that family caregivers spend an average of $7,200 per year of their own money on caregiving expenses (like medications, medical supplies, home modifications, transportation).
The emotional toll is impossible to measure, but very real. A significant number of working caregivers report job-related difficulties because of caregiving.
What the Caregiver Experience Actually Looks Like
Both hospital settings require serious caregiver involvement, just in different ways.
Caregiving during traditional hospitalization

You become an advocate and information manager. When doctors round at 8 a.m. and you can’t be there because you have a job, you miss critical conversations. So you take time off. You show up early. You stay late.
I kept notes from every specialist visit, cross-referenced medications, and flagged contradictions. The nutritionist told George to eat high-protein foods for his kidney disease. The renal dietitian told him to eat low-protein foods for his kidney disease. Guess who had to figure that out?
You’re also managing communication with the rest of the family. Who’s visiting when? Who needs updates? Coordinating schedules becomes a part-time job.
Caregiving with hospital at home

At home, you’re more hands-on with daily care:
- You help your loved one to the bathroom.
- You make sure they eat.
- You learn to manage medications (when to give them, and spot side effects)
The medical team trains you. They don’t just hand you a list of tasks and disappear. They show you how to help with care, what to watch for, and when to call for help.
When I was managing George’s peritoneal dialysis at home, his nephrologist’s team trained me thoroughly. I set up the machine every night, monitored the process, troubleshot issues.
It was a big responsibility, but I wasn’t alone. I had 24/7 access to the dialysis team by phone.
The benefits of hospital-at-home care:
- You have more control over the environment
- You can maintain some routine
- You sleep in your own bed
The stress of feeling “on call” is real, but many caregivers prefer it to feeling helpless in a hospital where they can’t be present all the time.
A 2018 study in JAMA Internal Medicine found that caregiver stress levels were actually lower in hospital-at-home programs, despite more hands-on responsibility, because caregivers felt more informed and empowered.
How to Know if Hospital at Home is Right for Your Situation
Hospital-at-home isn’t for everyone. Here’s how to figure out if it makes sense for you.
Medical eligibility criteria

Your condition needs to be serious enough to require hospitalization but stable enough to monitor at home. This includes conditions like:
- Pneumonia (non-ICU level)
- Heart failure exacerbations
- COPD flare-ups
- Cellulitis and other serious infections
- Certain post-surgical recoveries
You don’t qualify if you need ICU-level care, constant monitoring, or procedures that can only be done in a hospital. You also need to live within 30 minutes of the hospital in case you need emergency transfer.
Home environment assessment

You need a space for medical equipment, like a corner where an IV pole can stand and monitoring equipment can plug in.
If you’re taking advantage of telehealth, you’ll also need reliable internet for video visits and data transmission and a phone.
Safety matters too. Can you get to the bathroom safely? Are there trip hazards that could cause falls? A nurse will assess your home before admission to make sure it’s appropriate.
Insurance coverage check
Call your insurance company and ask these specific questions:
- “Do you cover hospital-at-home programs?“
- “What’s my co-pay compared to traditional hospitalization?”
- “Do I need pre-authorization?”
- “Which hospitals in my area participate in your hospital-at-home network?”
Get the answers in writing. Insurance representatives make mistakes, and you don’t want surprises later.
Family readiness factors
Someone needs to be home or nearby. Not necessarily 24/7, but available. The medical team handles the clinical care, but you need a person there to help with activities of daily living and to be present during visits.
Consider your other responsibilities:
- Do you have young kids?
- Other family members who need care?
- A job with no flexibility?
Be honest about your capacity. There’s no shame in saying traditional hospitalization is the better fit for your situation.
How to Access Hospital-at-Home Programs

Most doctors won’t automatically offer this option. You have to ask for it.
When your doctor says you need to be admitted, ask: “Am I eligible for a hospital-at-home program?” If they say they don’t know or haven’t heard of it, ask them to check. Many physicians are still learning about these programs.
Call your insurance company before admission if possible. Verify coverage and get any necessary pre-authorizations. Some programs accept patients directly from the emergency department, which can save you hours in the ER waiting room.
To find hospitals offering hospital-at-home in your area, check the Medicare website’s Hospital Compare tool or call hospitals directly and ask if they participate in hospital-at-home programs.
Questions to Ask Before You Decide

Before you commit to hospital-at-home, get clear answers to these questions.
For your medical team:
- “Am I medically stable enough for hospital-at-home?”
- “What happens if my condition gets worse at night or on weekends?”
- “How quickly can I be transferred to the hospital if needed?”
For the program coordinator:
- “How many times per day will someone visit me?”
- “Will I see the same nurses and doctors, or will it change?”
- “What equipment will be in my home, and who maintains it?”
For your insurance:
- “What will my total out-of-pocket cost be?”
- “How many days of hospital-at-home care are covered?”
- “Is there a limit to how many times I can use this benefit?”
For your family:
- “What will I be responsible for as a caregiver?”
- “What training will I receive?”
- “Who can I call when I’m overwhelmed or unsure?”
Get these answers before you decide. Understanding what you’re signing up for prevents surprises and helps you plan.
Making the Right Choice for Your Family
Hospital-at-home delivers the same quality of clinical care as traditional hospitalization—sometimes better.
But the right choice depends on your medical situation, your home environment, your insurance coverage, and your family’s capacity to help with care.
If George had the option for hospital-at-home care during his treatment, would it have changed the outcome? Probably not. His conditions were too complex and unstable.
But it would have changed our experience. Fewer nights in uncomfortable hospital chairs. More time in our own home. Better sleep for both of us. For the right patient and the right family, those differences matter tremendously.
Know that you have options. Ask questions and advocate for yourself. Don’t assume the hospital is the only place to receive acute care, because it’s not.
If you’re facing hospitalization decisions for yourself or a loved one, share this information with your family. Ask your doctor about hospital-at-home before admission. You might be surprised by what’s possible.
References
Bruce, G. (2025). House passes 5-year hospital-at-home extension. Becker’s Health IT. Retrieved from https://www.beckershospitalreview.com/healthcare-information-technology/digital-health/house-passes-5-year-hospital-at-home-extension/
Cryer, L., Shannon, S. B., Van Amsterdam, M., & Leff, B. (2023). Costs for Hospital at Home Patients Were 19 Percent Lower, With Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs, 42(6), 861-868. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22665835/
Dhaliwal, J.S., & Dang, A.K. (2024). Reducing Hospital Readmissions. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK606114/
Edgar, K., Iliffe, S., Doll, H. A., Clarke, M.J., Gonçalves-Bradley, D.C., Wong E., & Shepperd, S. (2024). Admission avoidance hospital at home. Cochrane Database of Systematic Reviews. Mar 5;3(3):CD007491. doi: 10.1002/14651858.CD007491.pub3. Retrieved from https://pubmed.ncbi.nlm.nih.gov/38438116/
Federman, A. D., Soones, T., DeCherrie, L. V., Leff, B., & Siu, A. L. (2018). Association of a Bundled Hospital-at-Home and 30-Day Postacute Transitional Care Program With Clinical Outcomes and Patient Experiences. JAMA Internal Medicine. Aug 1;178(8):1033-1040. doi: 10.1001/jamainternmed.2018.2562. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29946693/
HAI and Antimicrobial Use Prevalence Surveys. (2024). Centers for Disease Control. Retrieved from https://www.cdc.gov/healthcare-associated-infections/php/haic-eip/antibiotic-use.html
Horwitz, L. I., Moriarty, J. P., Chen, C., et al. (2020). Quality of discharge practices and patient understanding at an academic medical center. JAMA Internal Medicine, 180(8), 1125-1131. Retrieved from https://pubmed.ncbi.nlm.nih.gov/23958851/
Levine, D. M., Ouchi, K., Blanchfield, B., et al. (2023). Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Annals of Internal Medicine, 176(11), 1455-1466. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31842232/
Pollitz, K., Lopes, L., Kearney, A., Rae, M., Cox, C., Fehr, R., & Rousseau, D. (2019). An Examination of Surprise Medical Bills and Proposals to Protect Consumers from Them. Kaiser Family Foundation. Retrieved from https://www.kff.org/health-costs/an-examination-of-surprise-medical-bills-and-proposals-to-protect-consumers-from-them/
Reinhard, S. C., Caldera, S., Houser, A., & Choula, R. B. (2023). Valuing the Invaluable 2023 Update: Strengthening Supports for Family Caregivers. AARP. Retrieved from https://www.aarp.org/content/dam/aarp/ppi/2023/3/valuing-the-invaluable-2023-update.doi.10.26419-2Fppi.00082.006.pdf





































































.jpg?width=734&height=367)