As a caregiver, you may feel overwhelmed, isolated, or unsure where to turn for help. Community resources offer more than just emotional support–they’re lifelines that connect caregivers with others who truly understand their daily challenges. However, according to the National Alliance for Caregiving, only 28% of unpaid caregivers attend caregiver support groups.
Whether you’re caring for an aging parent, a child with special needs, or a spouse with a chronic illness, local support groups can provide the assistance, guidance, and emotional support you need to navigate your caregiving journey. We’ll explore the benefits of joining a support group, the types available, how to find them, and how to make the most of these valuable resources.
Contents
- Benefits of Joining a Local Caregiver Support Group
- Learn practical caregiving tips and strategies from experienced members
- Share experiences in a safe, judgment-free environment
- Access emotional support and validation from peers
- Discover local resources and services you might not know about
- Build lasting friendships with people who understand your situation
- Find respite care opportunities and backup support
- Types of Caregiver Support Groups Available
- How to Find Support Groups in Your Area
- Making the Most of Support Group Meetings
- Additional Support Resources for Caregivers
Benefits of Joining a Local Caregiver Support Group
Joining a local caregiver support group can be a game-changer for many caregivers.
Learn practical caregiving tips and strategies from experienced members
Support groups are a goldmine of practical knowledge. Caregivers who participate in support groups often improve their caregiving skills and knowledge. You’ll learn from others who have faced similar challenges and found effective solutions.
Share experiences in a safe, judgment-free environment
One of the most valuable aspects of support groups is the opportunity to share your experiences without fear of judgment. This can be incredibly cathartic and help reduce feelings of isolation, depression and anxiety.
Access emotional support and validation from peers

Caregiving can be emotionally taxing. Support groups provide a space where you can receive empathy and understanding from people who truly get what you’re going through. One study found that caregivers who attended support groups felt emotionally supported and less burdened (Wiegelmann et al., 2021).
Discover local resources and services you might not know about
Support group members often share information about local services, programs, and resources that can make caregiving easier. This network of shared knowledge can be invaluable in finding the right help for your specific situation.
Build lasting friendships with people who understand your situation

Many caregivers form deep, lasting friendships with fellow support group members. These connections can provide ongoing support and companionship beyond the group meetings themselves.
Find respite care opportunities and backup support
Support groups can be a great place to learn about respite care options in your area or even find other caregivers willing to provide backup support when you need a break.
Types of Caregiver Support Groups Available
Not all support groups are created equal. Here are some common types you may encounter.
Condition-specific groups
Some support groups focus on caregiving for specific conditions like kidney disease, cancer and autism, allowing members to share highly relevant experiences and information. For example, the Alzheimer’s Association offers support groups specifically for caregivers of individuals with Alzheimer’s and other dementias.
Age-based groups

Some groups are organized around the age of the care recipient, such as senior care or child care. This can be helpful as caregiving challenges often vary depending on whether you’re caring for an elderly parent or a child with special needs.
Relationship-based groups
These groups bring together caregivers who share similar relationships with their care recipients, such as spouse or adult children caregivers. For instance, a group for adult children caring for aging parents might address unique challenges like balancing work, family, and caregiving responsibilities.
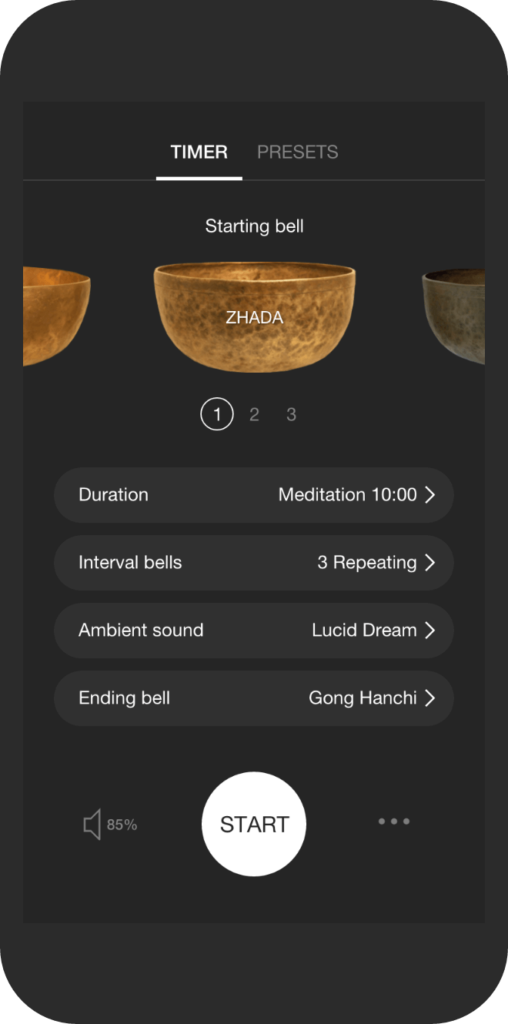
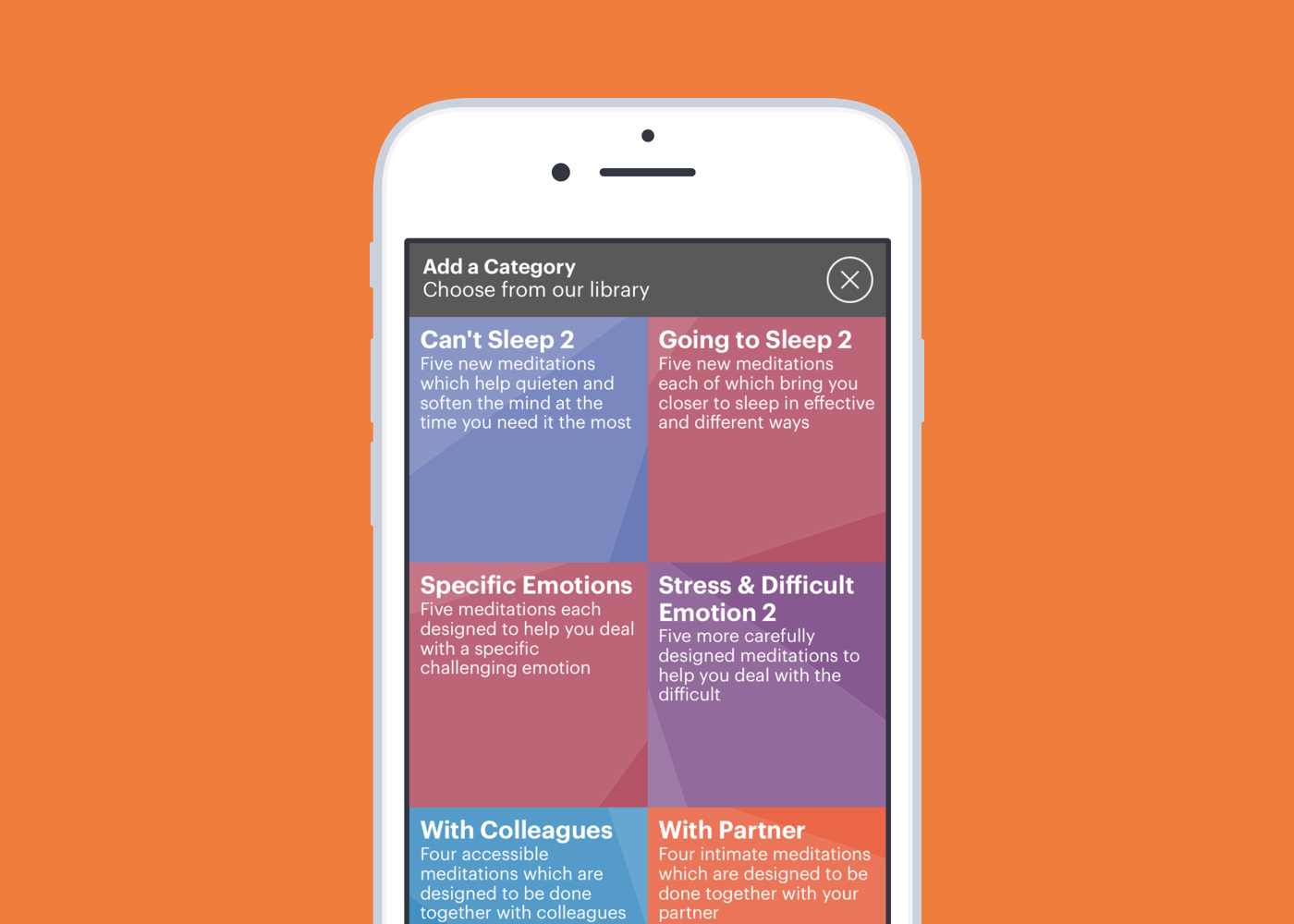
Online vs. in-person meeting options
With the rise of digital technology, many support groups now offer online options. A 2022 study in the found that online support groups can be just as effective as in-person groups in reducing caregiver stress and improving well-being (Egan et al., 2022).
Professional-led vs. peer-led groups

Some groups are led by healthcare professionals or social workers, while others are facilitated by experienced caregivers. Both can be beneficial, depending on your preferences and needs.
Specialized groups for working caregivers
These groups focus on the unique challenges faced by those balancing caregiving with employment. They often meet outside of typical work hours and address topics like managing time off and communicating with employers.
How to Find Support Groups in Your Area
Finding the right support group might take a bit of research, but it’s worth the effort. Here are some strategies to help you locate groups in your area.

Contact local hospitals and healthcare providers
Many hospitals and healthcare systems offer support groups for caregivers. Reach out to the social work department or patient services office for information.
Search online databases and directories
Websites like the Family Caregiver Alliance offer searchable databases of support groups across the country. Simply enter your location to find options near you.
Reach out to disease-specific organizations
Organizations focused on specific conditions often provide or can direct you to relevant support groups. For example, the American Cancer Society offers a database of cancer caregiver support groups.
Check with religious institutions and community centers
Many churches, synagogues, and community centers host caregiver support groups. These can be especially helpful if you’re looking for a group that aligns with your faith or cultural background.
Ask your doctor or healthcare team for recommendations

Your healthcare provider or your loved one’s medical team may be able to recommend local support groups that are relevant to your situation.
Use social media and local community forums
Platforms like Facebook and Nextdoor can be great resources for finding local support groups. Many groups have their own pages or groups where you can connect with other members.
A study conducted in Canada by Kelly et al (2022) looked at how caregivers of children with complex care needs used a private Facebook support group. The group had 108 members, mostly women. Many members belonged to multiple support groups, using each for different purposes.

The study found three key factors that made the group successful:
- Privacy was crucial. Because members came from a small geographic area, having a private group helped them feel emotionally safe sharing personal information.
- The group’s small size (under 150 members) and shared experiences helped build trust among members.
- Having active, knowledgeable moderators–including a healthcare professional and an experienced caregiver–helped keep the group engaged and reliable.
Even though most members were “lurkers” who rarely posted, they still benefited by reading others’ posts and searching for previous discussions about their concerns. The most common posts were questions, followed by information sharing and emotional support.
Many members felt motivated to help others by sharing their own experiences and knowledge. They viewed their lived experience as valuable information they could pass on to newer caregivers. While there were concerns about possible misinformation, having active moderators and members who could fact-check posts helped maintain accuracy in the group.
Making the Most of Support Group Meetings
Once you’ve found a support group, here are some tips to help you get the most out of your experience.

What to expect at your first meeting
You may feel a little uneasy attending your first meeting, but everyone there was new at first. Typically, you’ll be welcomed by the group leader, introduced to other members, and given an overview of how the group operates.
Tips for active participation
While it’s okay to simply listen at first, active participation can enhance your experience. Share your story when you feel comfortable, ask questions, and offer support to others when you can.
Set attendance goals
Consider what you hope to gain from the group and set some personal goals. This might include learning specific caregiving skills, finding emotional support, or connecting with local resources.
Balance sharing and listening

Support groups work best when there’s a balance between sharing your own experiences and listening to others. Be mindful of giving others a chance to speak and avoid dominating the conversation.
Build connections outside the group
Many caregivers find it helpful to connect with other group members outside of meetings. This can provide additional support and friendship.
Use group resources effectively
Many support groups offer resources like educational materials, guest speakers, or workshops. Take advantage of these opportunities to expand your knowledge and skills.
Additional Support Resources for Caregivers
While support groups are invaluable, they’re not the only resource available to caregivers. Here are some additional options to consider.

Professional counseling options
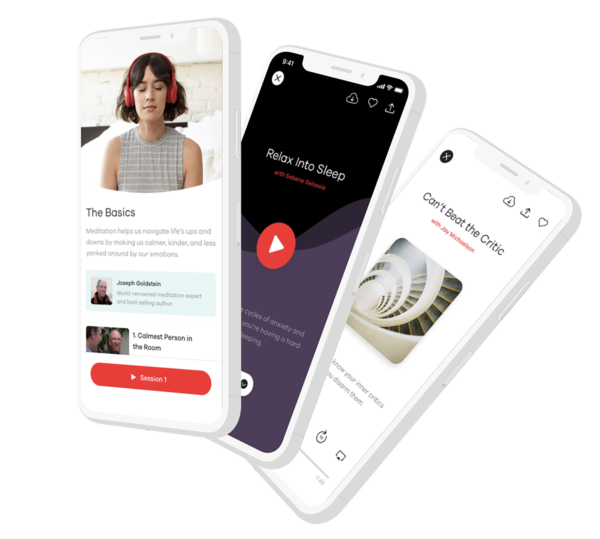
Individual or family counseling can provide personalized support for dealing with the emotional challenges of caregiving. Many therapists now offer telehealth options for added convenience.
Online forums and virtual communities
Websites like Caregiver.com and AgingCare.com offer online forums where caregivers can connect, share experiences, and seek advice.
Local respite care services

A study published in BMC Palliative Care revealed that family caregivers prioritize patient care but also need support for themselves. They want to be involved in care decisions and prepared for medical procedures. They also need recognition and respite to continue their caregiving duties (Nysaeter at al., 2024).
Respite care provides temporary relief for caregivers. Services can range from a few hours of in-home care to short-term stays at care facilities. The ARCH National Respite Network offers a locator tool to find services in your area.
Educational workshops and training
Many organizations offer workshops and training sessions for caregivers. For example, the National Alliance for Caregiving provides a variety of educational resources and webinars.
Financial assistance programs
Caregiving can be financially challenging. Programs like Medicaid waiver programs or veterans’ benefits may provide financial assistance. The National Council on Aging offers a Benefits CheckUp tool to help you find programs for which you may be eligible.
Emergency support services
It’s important to know what emergency support is available in your area. Many communities have crisis hotlines or emergency respite services for caregivers in urgent need of support.

Local caregiver support groups provide the understanding, resources, and community you need to thrive in your caregiving role. Don’t wait until you’re overwhelmed–reach out to find a group that fits your schedule and community resources that meet your needs.
These resources offer practical help, emotional support, and valuable connections that can make a world of difference in your caregiving journey. Take the first step to build your support network–your future self will thank you.
References
AgingCare.com. (2023). Caregiver Forum. Retrieved from https://www.agingcare.com/caregiver-forum
Alzheimer’s Association. (2023). Support Groups. Retrieved from https://www.alz.org/help-support/community/support-groups
American Cancer Society. (2023). ACS Patients Programs and Services. Retrieved from https://www.cancer.org/support-programs-and-services.html
ARCH National Respite Network and Resource Center. (2023). National Respite Locator Service. Retrieved from https://archrespite.org/respitelocator
Egan, K. J., Pinto-Bruno, Á. C., Bighelli, I., Berg-Weger, M., van Straten, A., Albanese, E., & Pot, A. M. (2022). Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: a systematic review. Journal of the American Medical Directors Association, 23(2), 217-226.
FCA CareJourney. (2023). Family Caregiver Alliance. Retrieved from https://www.caregiver.org/connecting-caregivers/services-by-state/
Kelly, K. J., Doucet, S., Luke, A., Azar, R., & Montelpare, W. (2022). Exploring the Use of a Facebook-Based Support Group for Caregivers of Children and Youth With Complex Care Needs: Qualitative Descriptive Study. JMIR Pediatrics and Parenting, 5(2), e33170. doi.org/10.2196/33170
National Alliance for Caregiving. (2023). Resources. Retrieved from https://www.caregiving.org/resources/
National Council on Aging. (2023). BenefitsCheckUp. Retrieved from https://benefitscheckup.org/
Nysaeter, T.M., Olsson, C., Sandsdalen, T., Hov, R., & Larsson, M. (2024). Family caregivers’ preferences for support when caring for a family member with cancer in late palliative phase who wish to die at home – a grounded theory study. BMC Palliative Care, 23, 15. doi.org/10.1186/s12904-024-01350-5
Support Groups. (n.d.) Family Caregiver Alliance. Retrieved from https://www.caregiver.org/connecting-caregivers/support-groups/
Wiegelmann, H., Speller, S., Verhaert, L. M., Schirra-Weirich, L., & Wolf-Ostermann, K. (2021). Psychosocial interventions to support the mental health of informal caregivers of persons living with dementia–a systematic literature review. BMC Geriatrics, 21(1), 1-17.