As women enter their midlife years, they often find themselves caught in the “sandwich generation,” caring for aging parents or family members while experiencing menopause. Over 60% of women experiencing menopause are also primary caregivers for a family member. The dual burden of caregiving during menopause can feel overwhelming, but with the right strategies, it’s possible to navigate both journeys successfully.
Contents
- The Challenges of Going Through Menopause While Caregiving
- Caregiver Burnout During Menopause
- Essential Self-Care Strategies for Menopausal Caregivers
- Creating Sustainable Caregiving Systems During Menopause
- Healthcare Considerations for Menopausal Caregivers
- Financial Planning During the Menopause and Caregiving Years
The Challenges of Going Through Menopause While Caregiving
Menopause is a natural biological process that marks the end of a woman’s reproductive years. During this time, the body undergoes significant hormonal changes that can affect various aspects of health and well-being. For women who are also caregivers, these changes can present additional challenges.
Hormonal changes affect energy and emotional resilience

The fluctuation and eventual decline of estrogen and progesterone levels during menopause can have a profound impact on energy levels and emotional stability. Many women report feeling more fatigued and less able to cope with stress during this time. This can be particularly challenging for caregivers, who often need to maintain high levels of energy and emotional resilience to meet the demands of their role.
The impact of caregiving during menopause

Menopausal symptoms can significantly affect a woman’s ability to provide care. Some of the most common symptoms include:
- Hot flashes and night sweats
- Sleep disturbances (insomnia,restless legs syndrome (RLS), sleep apnea)
- Mood changes, including irritability and anxiety
- Cognitive changes, such as “brain fog” (difficulty concentrating)
These symptoms can make it harder for caregivers to perform their duties effectively and may lead to increased stress and burnout. MayoClinic reported that caregiving for 15 hours or more each week makes menopause symptoms worse.
Statistics on menopausal caregivers
The overlap between menopause and caregiving is significant. According to a study published in Mayo Clinic Proceedings,19.7% of women aged 45-60 self-identified as caregivers. This age range coincides with the typical onset of menopause, which occurs around age 51 for most women in the United States.
Health consequences of neglecting self-cares
Neglecting self-care can have serious health consequences. Research has shown that caregivers who experience high levels of stress are at increased risk for various health problems, including heart disease, weakened immune function, gaining weight, and depression. When combined with the natural health risks associated with menopause, such as increased risk of osteoporosis and heart disease, the importance of self-care becomes even more critical.
Caregiver Burnout During Menopause
Caregiver burnout is a state of physical, emotional, and mental exhaustion that can occur when caregivers don’t get the help they need or try to do more than they’re able. During menopause, the risk of burnout may be even higher due to the added physical and emotional challenges women face.
Risks with caregiver burnout

Caregiver burnout is characterized by feelings of overwhelming exhaustion, detachment from the caregiving role, and a sense of hopelessness. During menopause, hormonal changes can amplify stress responses, making women more susceptible to burnout. The combination of caregiving duties and menopausal symptoms can create a perfect storm for physical and emotional depletion.
Warning signs specific to menopausal caregivers
While burnout can manifest in various ways, menopausal caregivers may experience some unique warning signs:
- Extreme fatigue that isn’t relieved by rest
- Increased irritability or mood swings
- Withdrawal from social activities and relationships
- Physical symptoms like headaches or digestive issues
- Difficulty managing menopausal symptoms
- Neglecting personal health and well-being
Hormonal fluctuations amplify stress responses
During menopause, fluctuations in estrogen and progesterone levels can affect the body’s stress response system. This can lead to an exaggerated reaction to stressors, making it harder for women to cope with the demands of caregiving. Additionally, the decline in estrogen can impact the production of stress-regulating neurotransmitters, potentially leading to increased anxiety and depression.
Importance of validating experiences and seeking support
Your experiences as a menopausal caregiver are valid and that seeking support is not a sign of weakness. Share their experiences with trusted friends, family members, or support groups specifically for menopausal caregivers.
Essential Self-Care Strategies for Menopausal Caregivers
Self-care is not a luxury for menopausal caregivers—it’s a necessity. Implement effective self-care strategies to help manage both your menopause symptoms and caregiver stress.
Hormone-balancing nutrition

A balanced diet can help alleviate some menopausal symptoms and provide the energy needed for caregiving. Consider the following nutritional strategies:
- Increase intake of phytoestrogens found in soy products, flaxseeds, and legumes
- Consume foods rich in calcium and vitamin D to support bone health
- Include omega-3 fatty acids from fish or supplements to support mood and cognitive function
- Limit caffeine, alcohol, and spicy foods that may trigger hot flashes
Exercise routines for menopause symptoms and caregiver stress

Regular physical activity can help manage both menopause symptoms and caregiver stress. Aim for a combination of:
- Aerobic exercise for heart health and mood improvement
- Strength training to maintain muscle mass and bone density
- Yoga or tai chi for stress reduction and balance
Sleep hygiene tips for menopausal caregivers

Quality sleep is essential for managing stress and hormonal changes. Try these sleep hygiene tips:
- Maintain a consistent sleep schedule
- Create a cool, dark sleeping environment
- Avoid screens before bedtime
- Practice relaxation techniques before sleep
Mindfulness and stress reduction techniques

Incorporating mindfulness practices into daily routines can help manage stress and improve emotional well-being. Consider:
- Short meditation sessions throughout the day
- Deep breathing exercises during caregiving tasks
- Mindful walking or other forms of moving meditation
Here’s some more ways to prevent burnout.
Creating Sustainable Caregiving Systems During Menopause
Developing sustainable caregiving systems is crucial for maintaining long-term health and well-being during menopause.
Communicate needs and limitations

Open communication with family members and care recipients is essential. Be honest about your capabilities and limitations, especially on days when menopause symptoms are particularly challenging. Use “I” statements to express your needs without placing blame, for example: “I need help with meal preparation today because I’m experiencing severe fatigue.”
Delegate caregiving tasks
Don’t hesitate to delegate tasks to other family members or professional caregivers. Create a list of tasks that can be shared and assign them based on individual strengths and availability. A study in The Gerontologist found that caregivers who shared responsibilities reported lower levels of stress and better mental health.
Building support networks and respite care options

Develop a strong support network that includes:
- Family members and friends
- Support groups for menopausal caregivers
- Professional respite care services
- Caregiver support groups
Regular respite care can provide much-needed breaks to reduce stress and help prevent burnout. .
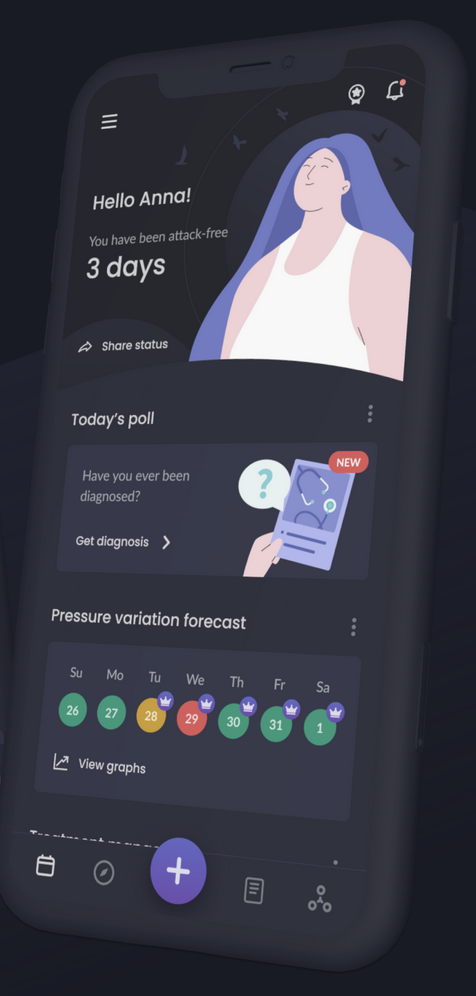
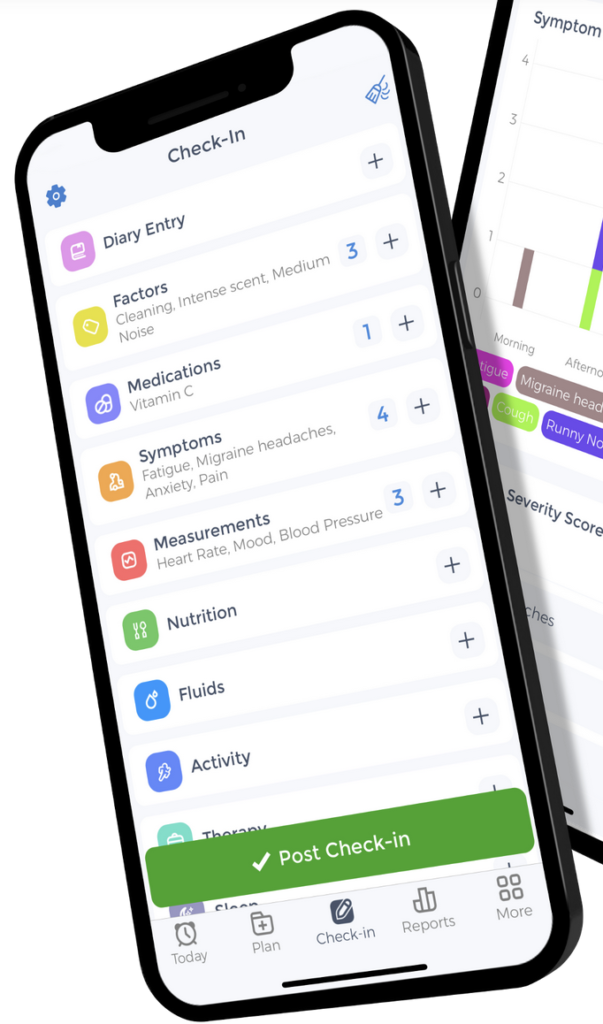
Digital tools and resources for efficient caregiving
Leverage technology to streamline caregiving tasks:
- Use medication reminder apps
- Implement smart home devices for safety monitoring
- Use care coordination platforms to manage schedules and tasks
Healthcare Considerations for Menopausal Caregivers
As a menopausal caregiver, it’s very important to make your personal health a priority to maintain your well-being and caregiving abilities.
Make and keep regular health appointments

Despite busy schedules, regular health check-ups are essential. These appointments provide opportunities to:
- Monitor menopause symptoms and overall health
- Discuss preventive care strategies
- Address any emerging health concerns
Questions to discuss with healthcare providers
Prepare a list of questions for your healthcare provider, such as:
- What treatment options are available for my specific menopause symptoms?
- How can I manage the stress of caregiving during menopause?
- Are there any screenings or preventive measures I should consider?
Check out this blog for more questions to ask them.
Treatment options compatible with caregiving duties

Discuss treatment options that fit your lifestyle as a caregiver:
- Hormone replacement therapy (HRT) if appropriate
- Non-hormonal medications for specific symptoms
- Lifestyle modifications and complementary therapies
When to seek additional support

Be aware of signs that indicate a need for additional support:
- Persistent feelings of sadness or anxiety
- Inability to perform caregiving duties
- Thoughts of self-harm or harming others
Financial Planning During the Menopause and Caregiving Years
Financial planning is a crucial aspect of managing the dual challenges of menopause and caregiving.
The impacts of caregiving on finances during menopause
Caregiving can have significant financial implications, including:
- Reduced work hours or early retirement
- Out-of-pocket expenses for care recipient needs
- Potential loss of savings or retirement funds
An AARP report found that family caregivers spend an average of $7,242 per year on out-of-pocket costs related to caregiving.
Healthcare coverage and benefits for caregivers

Explore available healthcare coverage and benefits:
- Review your health insurance policy for menopause-related treatments
- Investigate caregiver support programs offered by employers or local agencies
- Consider long-term care insurance for yourself and care recipients
Resources for financial planning
Utilize financial planning resources tailored to menopausal caregivers:
- Consult with a financial advisor experienced in caregiving issues
- Attend workshops on financial planning for caregivers
- Use online tools and calculators to assess financial needs
Work accommodations for menopausal caregivers

Discuss potential work accommodations with your employer:
- Flexible work hours to manage caregiving responsibilities
- Telecommuting options to balance work and care duties
- Employee assistance programs for counseling and support
A study in the journal Work & Stress found that flexible work arrangements (FWAs) are associated with reduced work-family conflict and improved well-being for caregivers.
You may also qualify for leave under the Family and Medical Leave Act (FMLA)—check with your employer, and learn about your rights under that law.
Finding harmony between the personal journey of menopause and the demands of caregiving requires intention, support, and compassion—especially for yourself. By implementing the strategies discussed in this guide, you can better manage your menopausal symptoms while continuing to provide quality care for your loved ones.
Taking care of your own health isn’t selfish—it’s essential for sustainable caregiving. Reach out to healthcare providers, support groups, and community resources to create a network that supports both your caregiving role and your personal well-being during this significant life transition.
References
Botek, A. Caregiving and Menopause: How to Handle the Double-Whammy. AgingCare. Retrieved from https://www.agingcare.com/Articles/handle-menopause-while-caregiving-153320.htm
Braun, N. (2024). Caring for Yourself While Caring for Others. Versalie. Retrieved from https://www.versalie.com/blogs/learn/caring-for-yourself-caring-for-others
Brown, R. M. (2024). There’s an App for That: Reducing Stress in Peri- And Post-Menopausal Women. Doctor of Nursing Practice Final Manuscripts. 285. doi.org/10.22371/07.2024.020
Bryan, L. & Dweck, A. (2024). How Can Menopause Affect Sleep. Sleep Foundation. Retrieved from https://www.sleepfoundation.org/women-sleep/menopause-and-sleep
Building a Network: The Social Benefits of Caregiver Support Groups. (2024). Trualta. Retrieved from https://www.trualta.com/resources/blog/building-a-network-the-social-benefits-of-caregiver-support-groups/
Building a Support Network: Finding Help as a Caregiver. (2024). Elder-Well Adult Day Program. Retrieved from https://elderwelladultday.com/building-a-support-network-finding-help-as-a-caregiver/
Caregiver Burnout. Cleveland Clinic. Retrieved from https://womenshealth.gov/a-z-topics/caregiver-stress
Caregiver stress. (2025). Office on Women’s Health. Retrieved from https://womenshealth.gov/a-z-topics/caregiver-stress
Crickmar, R. (2025). The Importance of Self-Care for Parents and Caregivers: Prioritizing Yourself To Support Your Family. Therapeutic Partners. Retrieved from https://therapeuticpartners.com/2025/02/06/the-importance-of-self-care-for-parents-and-caregivers-prioritizing-yourself-to-support-your-family/
Fatigue and menopause: tips to boost energy. (2024). Balance-Menopause. Retrieved from https://www.balance-menopause.com/menopause-library/fatigue-and-menopause-tips-to-boost-energy/
Hayes, J. & Rose, B. (2024). Caregiving as a Women’s Health Issue. NextAvenue. Retrieved from https://www.nextavenue.org/caregiving-as-a-womens-health-issue/
How expert financial advice can help to close the menopause retirement gap. (2024). Foster Denovo. Retrieved from https://www.fosterdenovo.com/how-expert-financial-advice-can-help-to-close-the-menopause-retirement-gap/
Li, Q. (2024). Sandwich caregiving and midlife women’s health: An examination of racial disparities. Family Relations, 73(5), 3291-3308. https://doi.org/10.1111/fare.13083
Menopause and money: Why financial planning is so important. (2024). RBC Brewin Dolphin. Retrieved from https://www.brewin.co.uk/insights/menopause-and-money-why-financial-planning-is-important
Menopause and the workplace. (2023). NHS inform. Retrieved from https://www.nhsinform.scot/healthy-living/womens-health/later-years-around-50-years-and-over/menopause-and-post-menopause-health/menopause-and-the-workplace/
Miller, H. (2024). Menopause & Stress. Dutch Test. Retrieved from https://dutchtest.com/articles/menopause-stress
Miller, S. (2024). From Hot Flashes to Health Costs: The Financial Impact of Menopause on Women. BayView Financial Planning. Retrieved from https://bayviewfp.com/from-hot-flashes-to-health-costs-the-financial-impact-of-menopause-on-women/
Newson, L. (2024). Coping with perimenopause when you’re a carer. Balance-Menopause. Retrieved from https://www.balance-menopause.com/menopause-library/coping-with-the-perimenopause-when-youre-a-carer
Prioritizing care for others, women often neglect their own health. (2020). American Heart Association. Retrieved from https://www.goredforwomen.org/en/beyond-the-table/stories/women-often-neglect-their-own-health
Saadedine, M., Safwan, N., Kapoor, E., et al. (2025). Association of Informal Caregiving and Menopause Symptoms in Midlife Women: A Cross-Sectional Study. Mayo Clinic Proceedings, 100(1), 42-51. Retrieved from https://www.mayoclinicproceedings.org/article/S0025-6196(24)00353-7/fulltext
Shakeel, W. (2024). Menopause Self Care: A Comprehensive Guide. Revive Research Institute. Retrieved from https://www.reviveresearch.org/blog/menopause-self-care
Shifrin, N. V., & Michel, J. S. (2021). Flexible work arrangements and employee health: A meta-analytic review. Work & Stress, 36(1), 60–85. doi.org/10.1080/02678373.2021.1936287
Snelling, S. (2015). When Menopause and Caregiving Collide. NextAvenue. Retrieved from https://www.nextavenue.org/when-menopause-and-caregiving-collide/
Skufca, L. (2021). Caregiving Can Be Costly – Even Financially. AARP. Retrieved from https://www.aarp.org/pri/topics/ltss/family-caregiving/family-caregivers-cost-survey/
Stress and your health. (2025). Office on Women’s Health. Retrieved from https://womenshealth.gov/mental-health/good-mental-health/stress-and-your-health
Taking Care of Yourself: Tips for Caregivers. (2023). National Institute on Aging. Retrieved from https://www.nia.nih.gov/health/caregiving/taking-care-yourself-tips-caregivers
Vazquez, E. K. (2025). The Impact of Hormones on Mental Health. Medens Health. Retrieved from https://www.medenshealth.com/blog/the-impact-of-hormones-on-mental-health



































.jpg?width=734&height=367)
















