The House spending bill dropped a bombshell for digital health companies: a proposed 5-year extension for hospital-at-home waivers and 2-year extension for Medicare telehealth flexibilities.
Five years sounds like forever in tech time. But it’s actually a strategic planning nightmare.
Do you build for temporary policy, or bet everything on permanence?
I spent 2 years managing care for my terminally ill husband across 10 different doctors. Every month, he landed back in the hospital with high A1C, low hemoglobin, unbearable pain. If hospital-at-home programs had existed in 2016 with the right technology backing them, he could have avoided dozens of ER visits.
Hospital at home is the future. The question is, what should Series A, B and C health tech founders build in the next 24 months that creates value regardless of what Congress does in 2030?
This isn’t about policy speculation. It’s about strategic planning with incomplete information—which is exactly what building a health tech company requires.
Let’s break down the roadmap.
Contents
- What the Proposed Funding Package Actually Changes
- Most Founders Are Asking the Wrong Question
- Your 24-Month Minimum Viable Stack
- The Margin Math That Actually Matters
- The 3 to 5 Year Platform Expansion Strategy
- Decision Framework for Health Tech Boards
- What I Wish Existed When I Was a Caregiver
- The Path Forward
What the Proposed Funding Package Actually Changes

The proposed House spending bill extends two critical Medicare programs—but on very different timelines. Understanding these differences matters if you’re building technology in this space.
The 5-year hospital-at-home timeline explained
The proposed legislation would extend the hospital-at-home waiver through 2030. This isn’t just another short-term patch. Previous extensions gave health systems and tech companies 12-18 months of runway at best.
The current acute hospital care at home initiative lets Medicare pay for hospital-level services delivered in patients’ homes. Without the extension, this program expires in 2025. That’s not enough time to build, validate, and scale meaningful technology infrastructure.
Five years gives you real planning horizon. You can make legitimate platform investments. You can hire engineering teams. You can sign multi-year contracts with health systems.
But—and this is critical—5 years isn’t permanent. It’s a policy experiment with a longer fuse.
What’s still uncertain despite the extension

Even with a 5-year extension, huge questions remain unanswered. CMS hasn’t committed to specific reimbursement rates beyond the waiver period. Will hospital-at-home payments match facility-based acute care, or will they drop to home health rates?
State regulations vary wildly. Some states embrace home-based acute care. Others have licensing requirements that make it nearly impossible. Federal waivers don’t override state-level barriers.
Commercial payers watch Medicare but don’t automatically follow. Your hospital-at-home technology needs Medicare coverage to scale, but commercial adoption determines whether you build a sustainable business.
Technology requirements could shift too. CMS might mandate specific monitoring capabilities, interoperability standards, or quality reporting metrics that don’t exist yet.
Planning for 5 years means planning for uncertainty, not betting on stability.
Most Founders Are Asking the Wrong Question
When the House bill news broke, founder group chats exploded with one question: “Does this mean hospital-at-home is permanent?” That’s the wrong question. It reveals a misunderstanding of how health tech businesses actually succeed or fail.
“Is this permanent?” misses the strategic point
Policy permanence has never guaranteed health tech success. Remote patient monitoring has had Medicare coverage since 2019. Chronic care management codes have existed for years. Both have clear reimbursement pathways. Both have policy stability.
Yet most RPM companies struggle to achieve profitability. Many CCM platforms shut down despite favorable policy.
The real risk isn’t policy reversal. It’s building something nobody needs or can’t afford to operate. Investors price in regulatory risk and execution challenges unique to healthcare.
Your business model needs to create value across multiple scenarios. If hospital-at-home waivers expire in 2030, can your technology pivot to post-acute care? Skilled nursing facilities? Palliative care at home? If you’ve built exclusively for one reimbursement code, you’ve built a fragile company.
The trap of building exclusively for waivers

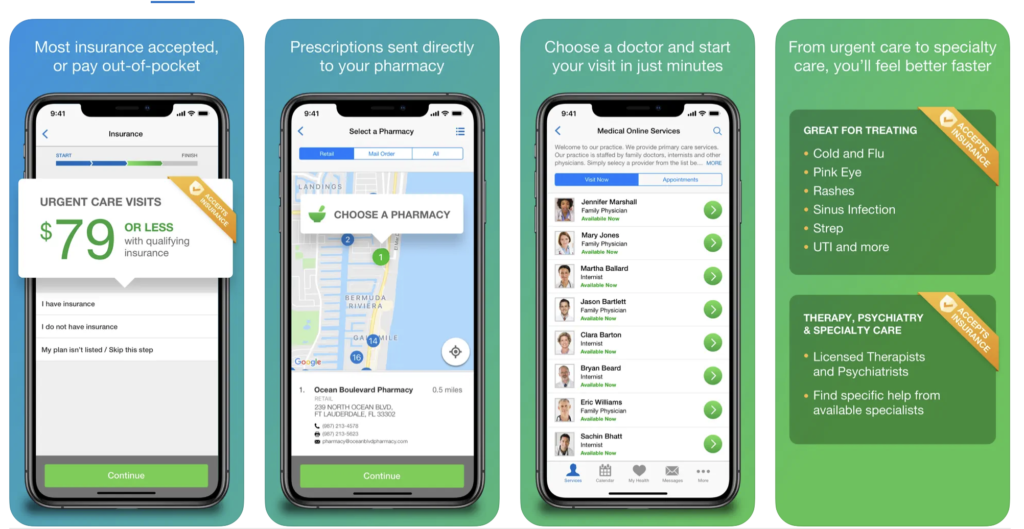
Remember the telehealth boom of 2020-2021? Some telehealth companies that scaled to thousands of employees during COVID laid off half their staff by 2023.
They weren’t bad companies. They built for a policy moment, not a durable market need.
VCs learned an expensive lesson: waiver-dependent revenue is risky revenue. When I talk to Series B investors now, they ask pointed questions. What percentage of your revenue requires temporary policy? If that policy changes, what’s your Plan B? Can you operate profitably under traditional Medicare rates?
If you can’t answer those questions convincingly, your valuation suffers—even if current policy looks favorable.
What “5 years” really means for your product roadmap
Five years is approximately two technology development cycles for complex healthcare platforms. You can ship an MVP, gather real-world evidence, iterate based on feedback, and launch a mature v2.0 product in that timeframe.
But 5 years isn’t enough time to build everything. You need to prioritize ruthlessly.
Your 24-month window is critical. This is when you validate product-market fit, prove unit economics, and establish your competitive moat. If you can’t demonstrate margin-positive cohorts by month 24, the next 3 years won’t save you.
Years 3 to 5 should assume policy uncertainty, not stability. Build optionality into your architecture. Make sure your platform can serve multiple care settings. Design your data infrastructure to support different payment models.
One scenario planning exercise: map out what your business looks like if hospital-at-home waivers expire in 2030 versus extend another 5 years vs. become permanent. If all three scenarios require fundamentally different strategies, you’re not building a durable company. You’re building a policy bet.
Your 24-Month Minimum Viable Stack

The next 2 years determine everything. You need to build technology that proves value quickly while laying foundation for longer-term expansion. Here’s where to focus your engineering resources and capital.
Core infrastructure that works across reimbursement models
Start with the basics that every home-based care model needs, regardless of how Medicare pays for it.
Remote patient monitoring devices need to integrate seamlessly with your platform. But don’t overbuild here. Start with FDA-cleared devices for vital signs (blood pressure, pulse ox, weight, glucose). Specialty monitoring for rare conditions can wait until you’ve proven your core model works.
Virtual triage and clinical communication platforms matter more than most founders realize. When a patient’s oxygen saturation drops at 3 a.m., someone needs to decide: send an ambulance, dispatch a nurse, or coach the patient through the moment remotely? That decision-making capability is what health systems pay for, not just the device data.
Care orchestration is the unsexy backbone nobody wants to build but everyone needs. Who schedules the nurse visit? Who orders medical supplies? Who coordinates with the patient’s primary care doctor? These back-office functions represent over half of the $1 trillion in annual U.S. healthcare waste. Automating them creates immediate ROI.
EHR integration isn’t optional. Payers demand it. Health systems require it. Your platform needs to pull patient data from Epic, Cerner, and other major EHRs, then push back visit notes, monitoring data, and care plans. Budget 20 to 30% of your engineering resources just for integration work.
Where to invest in AI right now

Ambient clinical intelligence (ACI) has reached near-universal adoption: 92% of health systems are piloting or deploying AI scribes. These tools improve documentation accuracy, leading to 10 to 15% revenue capture improvement through better coding and billing.
For hospital-at-home programs, this matters enormously. Nurses and paramedics doing home visits often struggle with documentation. They’re managing complex patients in unpredictable environments. AI that turns their verbal notes into structured clinical documentation saves 30 to 45 minutes per visit.
Predictive analytics should focus on preventing acute episodes that require hospitalization. Machine learning models can analyze vital sign trends, medication adherence patterns, and social determinants data to flag patients at risk of decompensation. One health system using predictive monitoring reduced readmissions by 23% in their hospital-at-home cohort—that’s the difference between a margin-positive program and one that loses money on every patient.
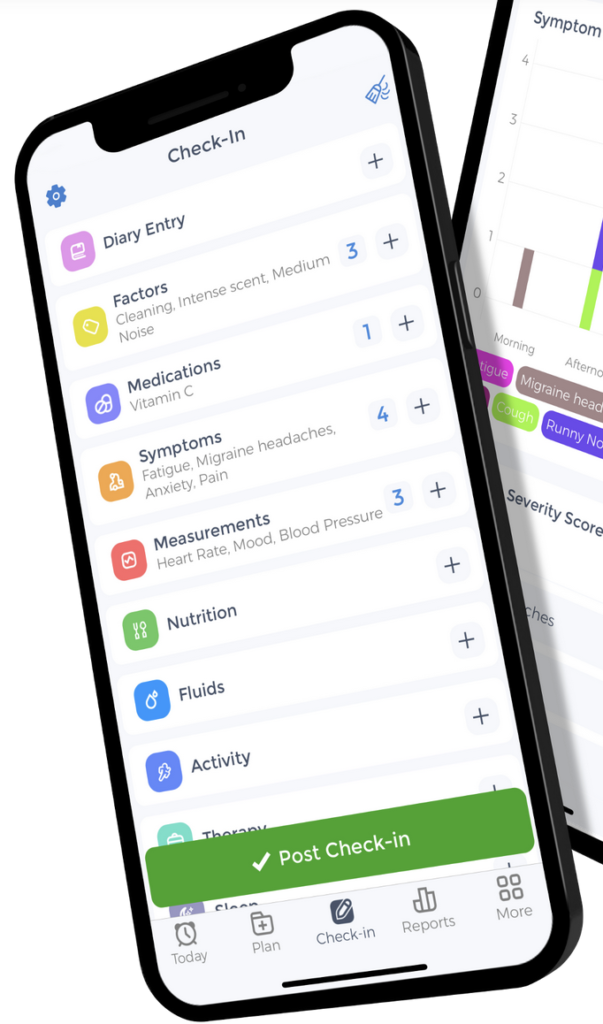
Don’t sleep on care coordination automation. If family caregivers spend 15-20 hours per week on caregiving tasks (as CareYaya Health Technologies data shows), your AI should reduce that burden. Automated medication reminders, appointment scheduling, and supply ordering aren’t flashy features, but they’re what caregivers desperately need.
The unsexy AI that saves money: Back-office automation in revenue cycle management, prior authorization, and claims integrity. These AI applications can reach 70-80% profit margins and generate $500K-$1M in annual recurring revenue per full-time employee. That cash flow funds your clinical AI development.
The Margin Math That Actually Matters

Most hospital-at-home programs lose money. Your technology needs to change that equation, or you don’t have a sustainable business.
Why most hospital-at-home programs lose money
Medicare pays $1,000 to $1,500 per day for hospital-at-home. Most programs spend $1,200 to $1,600 per patient daily on nurse visits, supplies, coordination, and tech. They’re underwater from Day 1.
The hidden costs kill you. Logistics and care orchestration require significant labor. Someone schedules visits, manages the supply chain, and coordinates with the patient’s other providers. Traditional staffing models don’t scale—you can’t apply facility-based nursing ratios to home care and expect it to work economically.
Technology that creates work instead of reducing it makes the problem worse. I’ve seen hospital-at-home platforms that require nurses to log into five different systems per visit. The documentation burden exceeds what they’d do in a hospital setting.
How AI makes care at home programs profitable
Revenue cycle optimization through better documentation can improve revenue capture by 10-15%. When a nurse describes a patient’s condition verbally and AI generates accurate, complete clinical notes with proper billing codes, you get paid more for the same work.

Reduced readmissions drive CMS quality bonuses. The hospital-at-home model already shows lower readmission rates than traditional acute care—adding predictive monitoring amplifies that advantage. Every readmission you prevent saves $10,000 to $15,000 in costs and protects against CMS penalties.
Labor cost reduction matters most. AI triage can cut nurse workload by 40%+ in pilot programs. Instead of nurses manually reviewing monitoring data for every patient, AI flags only the patients who need clinical attention. A nurse who previously managed 5-6 hospital-at-home patients can now manage 8 to 10.
The “unsexy” AI that CFOs love but VCs overlook: billing, coding, claims integrity. Administrative AI can reduce operational costs by 30-40%. That’s real margin improvement hitting your income statement immediately.
Proving ROI to your board in the next 6 months

Your board doesn’t care about utilization growth if you’re losing money on every patient. They care about these metrics:
- Cost per episode: What does it actually cost you to manage one hospital-at-home patient from admission to discharge? Track this ruthlessly. Break it down by component: labor, supplies, technology, overhead.
- Readmission rates: Hospital-at-home programs typically achieve 8 to 12% 30-day readmission rates versus 15 to 18% for traditional hospital care. If your program doesn’t beat facility-based benchmarks, you have a quality problem.
- Patient satisfaction: CMS increasingly ties reimbursement to patient experience scores. Hospital-at-home programs score 15-20 points higher on patient satisfaction versus facility care. That’s your competitive advantage.
Structure pilot programs that generate defensible data. Work with 2 to 3 health systems willing to share financial and outcomes data transparently. You need to prove your technology improves margins, not just clinical outcomes.
The difference between utilization metrics and profitability metrics: lots of patients using your platform means nothing if each one loses money. Focus on contribution margin per patient. When does that number go positive? What’s the path to 40 to 50% gross margins?
The 3 to 5 Year Platform Expansion Strategy
Once you’ve proven your core model works and generates positive margins, you can think bigger. The next phase is about expanding beyond your initial use case.
From point solution to platform
Bessemer’s State of Health AI report describes “supernova” companies that achieve 6-10x growth trajectories by expanding from single point solutions into comprehensive platforms. Ambient scribes became full clinical documentation suites. Prior authorization tools became complete utilization management platforms.
The pattern:
- Start with a painful, well-defined problem.
- Solve it better than anyone else.
- Expand into adjacent workflows that touch the same users.
For hospital-at-home technology, that might mean starting with post-surgical patients recovering at home. Prove you can manage that population safely and profitably. Then expand to heart failure management, COPD exacerbations, cellulitis treatment, chemotherapy administration.
Each expansion requires clinical validation and new reimbursement navigation. But your core technology infrastructure of monitoring, triage, care coordination, documentation stays largely the same.
Value-based care integration timeline

Hospital-at-home is a wedge into value-based care contracts, not just fee-for-service reimbursement. Accountable Care Organizations (ACOs) and Medicare Advantage plans care deeply about reducing avoidable hospitalizations. If your platform keeps patients out of expensive facility-based care, ACOs will pay for it.
But commercial adoption lags Medicare by 18 to 24 months historically. Don’t expect widespread MA plan adoption until 2027 to 2028, even with favorable hospital-at-home policy.
Self-insured employers represent a faster path to commercial revenue. Large employers pay directly for employee healthcare. When they see data showing hospital-at-home reduces costs by 30-40% versus facility admissions, they’ll write checks. Companies like Cubby, who secured $63 million in Series A funding led by Guggenheim Partners, are targeting this employer market specifically for in-home care solutions.
To position for risk-bearing contracts in years 3 to 5, you need data infrastructure now. Start collecting outcomes data, cost data, and patient experience data from day one. Value-based contracts require you to prove your intervention changes total cost of care—not just that patients like your service.

Decision Framework for Health Tech Boards
If you’re a founder presenting hospital-at-home strategy to your board, or a board member evaluating your company’s approach, here are the right questions to ask.
5 questions your board should ask right now
- What percentage of our revenue depends on waiver-specific reimbursement? If it’s above 50%, you have concentration risk. Diversify your payer mix and care settings.
- If the waiver expires in 5 years, what’s our Plan B business model? You should have a concrete answer. Can you pivot to post-acute care? Palliative care? Chronic disease management? If the answer is “we’re screwed without waivers,” you’re not building a durable company.
- Are we building technology that creates value in multiple care settings? The best health tech platforms work across hospital-at-home, skilled nursing, home health, and ambulatory settings. Flexibility equals durability.
- How quickly can we prove margin-positive unit economics? If you can’t show positive contribution margin by month 24, extending the timeline to month 36 won’t magically fix the problem. You have a business model issue, not a scale issue.
- What’s our competitive moat if 10 other startups get this same 5-year runway? Policy tailwinds create competition. What’s your defensible advantage? Clinical outcomes data? Payer relationships? Technology that’s genuinely better, not just first to market?
Investor perspective on policy-dependent businesses

VCs underwrite regulatory risk by discounting valuations and requiring faster paths to profitability. A pure software company might get 7-10 years to reach profitability. A health tech company with policy dependency gets 3-5 years maximum.
The valuation discount for waiver-dependent revenue can be brutal. Health tech companies trade at 10-20% below cloud software comparables—and that’s before factoring in temporary policy risk.
Some investors love policy tailwinds. They want to ride the wave while it’s building. Others avoid policy-dependent businesses entirely, no matter how attractive the market opportunity looks.
Position your pitch carefully. Are you policy-enabled (taking advantage of favorable reimbursement to scale faster) or policy-dependent (can’t exist without specific waivers)? The former gets funded at reasonable valuations. The latter struggles.
What I Wish Existed When I Was a Caregiver
Let me bring this back to why any of this matters. The technology decisions health tech founders make over the next 24 months will determine what tools families like mine have access to in 2026 and beyond.
The gap between technology capability and real-world reliability

My husband’s Dexcom continuous glucose monitor worked beautifully—when it synced properly. The app sent alerts to my phone whenever his blood sugar went dangerously high or low. That device probably saved his life multiple times.
But it only worked because the technology was reliable:
- The sensor stayed attached.
- The Bluetooth connection held.
- The app didn’t crash.
I’ve seen hospital-at-home platforms that look impressive in demos but break under real caregiver stress. The dashboard shows beautiful data visualizations—but requires three different logins to access. The monitoring devices pair easily in the clinic—but fail when WiFi is weak in rural areas.
Care coordination platforms often assume 24/7 nurse availability. They don’t account for the reality that small hospital-at-home programs can’t staff round-the-clock coverage.
Build for the worst-case scenario, not the ideal one.
Building for the sandwich generation managing multiple conditions

My husband had 10 doctors. Ten! A primary care physician, nephrologist, endocrinologist, oncologist, cardiologist, and five other specialists. Your platform needs the capability to handle that complexity.
Nobody coordinated between them. I was the coordination layer. I maintained a spreadsheet with all his medications—drug names, dosages, prescribing doctors, reasons for taking them, refill schedules. The nurses loved my spreadsheet because their systems couldn’t give them the same view.
Insurance coordination created endless frustration. My employer’s insurance was primary while Medicare was secondary. Every billing department called me multiple times to confirm this. I explained the same thing to the hospital billing office, the lab, the imaging center, the pharmacy.
Your hospital-at-home platform should automate this nightmare. Pull medication lists from multiple prescribers. Flag potential drug interactions. Coordinate insurance claims automatically. Don’t make family caregivers become project managers.
Why I care about this 5-year window
Families like mine in 2026 deserve better than what I had in 2016.
The technology exists now, and the clinical models work. The question is implementation and sustainability.
Health tech founders have a moral obligation beyond shareholder returns. Yes, you need to build a profitable business and generate returns for your investors. But you’re also building tools that will serve people during the most vulnerable moments of their lives.
This isn’t about making a quick buck off temporary Medicare waivers then exiting before they expire. It’s about building something that lasts. Something that works. Something that actually helps families manage impossible complexity.
When you’re making technology decisions over the next 24 months, remember: real people will rely on what you build. Build something worthy of that trust.
The Path Forward
The proposed 5-year extension for hospital-at-home waivers isn’t a guarantee. It’s a window.
What you build in the next 24 months determines whether your company survives beyond 2030—regardless of what happens with federal policy.
The smartest founders build technology that creates value across multiple reimbursement scenarios. Focus on margin-positive unit economics. Solve real problems for real families—the kind of problems I faced as a caregiver managing impossible complexity across disconnected systems.
- Start with the unsexy AI that makes programs profitable: revenue cycle management, clinical documentation, coding accuracy. These aren’t sexy pitch deck slides, but they generate cash flow.
- Build your minimum viable stack around care orchestration and monitoring that works when human resources are constrained. Health systems can’t hire infinite nurses. Your technology needs to make existing staff dramatically more productive.
- Structure pilot programs that generate defensible ROI data within 6 months. You need proof points for your next fundraise and for health system expansion.
- Stress-test your business model. If hospital-at-home waivers expire in 2030, what’s Plan B? If you don’t have a good answer, you’re building on quicksand.
Five years is enough time to build something durable if you start with the right foundation. It’s not nearly enough time if you’re building for a policy moment instead of a market need.
The families who need hospital-at-home can’t wait for perfect policy clarity. They need technology that works today and keeps working tomorrow. So build for that reality.
Want to discuss your hospital-at-home technology strategy? Connect with me on LinkedIn or explore more health tech analysis at reewrites.com.
References
Bessemer Venture Partners. (2026). State of Health AI 2026. Retrieved from https://www.bvp.com/atlas/state-of-health-ai-2026
Fox, A. (2026). 2026 House spending bill proposes 2-year telehealth and 5-year hospital-at-home waiver extensions. Healthcare IT News. Retrieved from https://www.healthcareitnews.com/news/2026-house-spending-bill-proposes-2-year-telehealth-and-5-year-hospital-home-waiver-extensions
Gardner, S. & Hooper, K. (2026). Health tech panel to reboot after a long break. Politico Pulse. Retrieved from https://www.politico.com/newsletters/politico-pulse/2026/01/21/health-tech-panel-to-reboot-after-a-long-break-00737790
Gonzales, M. (2026). Proposed Funding Package Would Extend Hospital-at-Home Program, Medicare Telehealth Flexibilities. Home Health Care News. Retrieved from https://homehealthcarenews.com/2026/01/proposed-funding-package-would-extend-hospital-at-home-program-medicare-telehealth-flexibilities/
Stock Titan. (2026). Cubby secures $63 million in Series A funding round led by Growth. Retrieved from https://www.stocktitan.net/news/GS/cubby-secures-63-million-in-series-a-funding-round-led-by-growth-ikgye2ab40md.html
Zanchi, M. G. (2026). AI Journal. The “unsexy” revolution within healthcare AI. Retrieved from https://aijourn.com/the-unsexy-revolution-within-healthcare-ai/