Pain is more than just a physical sensation—it’s a complex experience that can dramatically alter your daily life. Chronic pain affects almost 33% of adults, impacting their quality of life and daily activities. As traditional pain management methods often fall short, wearable pain management technologies offer hope for anyone struggling with ongoing pain.
These smart devices can:
- Track pain signals
- Provide quick relief
- Help you understand your pain better
Let’s see how.
Contents
Chronic Pain and Wearable Technologies

Types of chronic pain and pain conditions
Chronic pain can stem from various conditions, each presenting unique challenges:
- Fibromyalgia
- Lower back pain
- Multiple sclerosis (MS)
- Rheumatoid arthritis
- Neuropathic pain
- Endometriosis
- Migraines

Along with different conditions that cause chronic pain, there are different types of chronic pain:
- neuropathic (nerve) pain – related to nerve damage
- nociceptive pain – pain caused by an injury, inflammation, or pressure
- somatic pain – pain that starts in your face, limbs, or muscles
- visceral pain – pain from the internal organs with sensory nerves
Problems with traditional pain management

Traditional pain treatments often rely on medications, physical therapy, and lifestyle modifications. However, these methods have drawbacks:
- Medication side effects
- The risk of addiction
- Inconsistent pain relief
- Lack of personalization (one-size-fits-all approach)
Only about 17% of people living with chronic pain get enough pain relief from traditional treatments.
For example, Non-steroidal anti-inflammatory drugs (NSAIDs) have limited effectiveness in treating chronic pain and carry potential serious adverse effects, including an increased risk of heart attack or stroke. Opioids can be effective for short-term pain relief, but they have limited long-term effectiveness, and carry significant risks of addiction and misuse.
How wearable technologies detect and address pain
Wearable technologies offer a new approach to pain management:
- Monitor physiological (body) signals continuously
- Provide real-time pain relief
- Track pain patterns and triggers
- Offer personalized treatment options
A study published in the Interactive Journal of Medical Research reported that wearable devices improved pain management.
The science behind targeted pain relief

Wearable pain management devices use various scientific principles to provide targeted relief:
One example is Transcutaneous Electrical Nerve Stimulation (TENS), which works to reduce nociceptor activity and unwanted pain sensations.
Research from NXSTIM demonstrated that its TENS wearable device EcoAI reduced pain intensity for 92% of study participants.
Patient-reported outcomes and effectiveness
Wearable pain management technologies have shown promising results in patient-reported outcomes:
- Improved pain control
- Reduced medication use
- Enhanced quality of life
- Increased physical activity
A study on Spinal Cord Stimulation (SCS) therapy showed significant improvements in pain intensity and quality of life.
Types of Wearable Pain Management Devices
The market for wearable pain management devices has expanded rapidly, offering various options for different kinds of pain and patient needs.
Transcutaneous electrical nerve stimulation (TENS) devices

TENS devices use low-voltage electrical currents to provide pain relief. These wearable units typically consist of:
- A small, battery-powered device
- Electrode pads
- Adjustable intensity settings
The FDA approved the TensWave pain relief device, designed to be portable and user-friendly, to alleviate pain without medication.
Compression and support wearables

Compression garments and support devices can be helpful for conditions like arthritis or sports-related injuries. They help manage pain by:
- Improving blood circulation
- Reducing inflammation
- Providing joint stability
Research in the Arthritis Research and Therapy showed that a soft knee brace helped reduce pain, improve walking speed, and increase confidence for people with knee osteoarthritis.
Smart patches and biosensors

These advanced wearables use technology to:
- Monitor physiological signals
- Detect pain patterns
- Deliver targeted pain relief
For example, a DGIST research team has developed a smart patch capable of real-time biometric signal monitoring and drug delivery. This level of continuous monitoring and immediate response is impossible with traditional pain management methods.
Electromagnetic therapy devices

Electromagnetic therapy wearables use pulsed electromagnetic fields (PEMF) to:
- Reduce inflammation
- Promote tissue healing
- Alleviate pain
These devices can be effective for conditions like chronic lower back pain. Research has found that PEMF therapy reduced chronic lower back pain intensity in study participants.
Neurostimulation wearables

These devices target specific nerves to interrupt pain signals and provide relief. They can be used for various chronic pain conditions, including:
- Migraine headaches
- Neuropathic pain
- Fibromyalgia
A narrative review reported that a neurostimulation device reduced migraine pain within two hours.
Technology Behind Pain Relief Wearables
The effectiveness of wearable pain management devices relies on advanced technologies that work together to detect, analyze, and address pain.
Sensor technologies and pain detection

Wearable sensors measure body signals to understand how each person experiences pain. This helps create personalized pain treatment plans.
Wearable devices use various sensors to monitor physiological signals associated with pain:
- Accelerometers
- Heart rate monitors
- Skin conductance sensors
- Temperature sensors
AI-powered devices are changing how we handle pain. They use sensors to track pain signals in the body, along with AI algorithms to figure out the best way to treat each person’s pain. These tools can measure things like heart rate and skin changes to understand pain levels and suggest personalized treatments.
Electrical stimulation mechanisms

Electrical stimulation devices work by:
- Blocking pain signals
- Stimulating endorphin release
- Improving local blood circulation
Research published in the Scientific Reports showed that electrical stimulation wearables reduced chronic pain and improved the walking gait of participants.
Biofeedback and pain tracking
Biofeedback is a method that helps you learn more about how your body works. By using special electronic devices, you can track things like your heart rate, muscle tension, or breathing. The main goal is to teach you how to control these body functions on purpose, almost like learning to control a muscle you didn’t know you could move before.
Biofeedback features in wearable devices help patients:
By providing real-time feedback on physiological responses, these devices can empower you to take a more active role in managing your pain.
Machine learning and personalized pain management
AI and machine learning algorithms enhance the effectiveness of wearable pain management devices by:
- Analyzing individual pain patterns
- Predicting pain episodes
- Optimizing treatment parameters
For instance, a study on digital biomarkers collected from wearables during SCS treatment showed that machine learning models can predict pain levels with an accuracy of 76.8%.
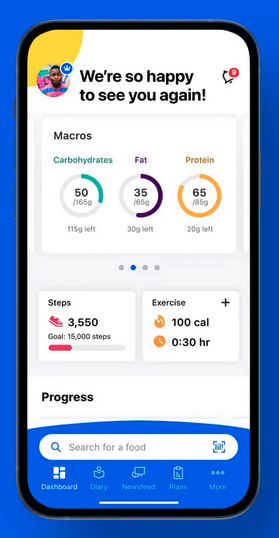
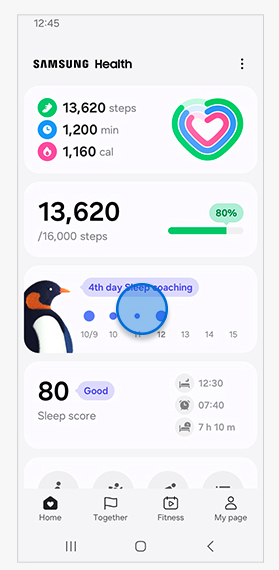
Integration with smartphone applications

Most wearable pain management devices connect to smartphone apps, offering:
- Real-time pain tracking
- Treatment customization
- Data sharing with healthcare providers
In one study, a pain management app helped participants track and manage chronic pain. Those experiencing higher pain intensity and disability found it the most valuable. Some users appreciated the tracking features, while others found frequent monitoring intrusive.
Integrating apps into your healthcare regime promotes more comprehensive pain management and better communication between you and your healthcare team.
Clinical Applications and Research
Wearable pain management technologies have shown promise in various clinical settings and for different types of pain.
Pain management for specific conditions

Researchers have studied wearable devices to see how effective they are when managing pain associated with:
- Fibromyalgia
- Osteoarthritis
- Lower back pain
- Neuropathic pain
For example, a study on SCS therapy showed significant improvements in pain intensity and quality-of-life metrics for people with chronic pain conditions.
Sports injury recovery

Athletes and sports medicine professionals turn to wearable pain management devices for:
- Faster recovery from injuries
- Reduced reliance on pain medications
- Improved rehabilitation outcomes
Compression wearables for instance, have shown promise in reducing pain and improving function in patients with knee osteoarthritis.
A study in BMC Sports Science, Medicine and Rehabilitation used advanced tracking devices like accelerometers, GPS, and force plates to monitor athletes’ performance. By collecting data on things like distance, speed, and impact, coaches can spot early signs of fatigue and prevent injuries. The technology can help sports coaches decide when to push athletes harder, and when to let them rest.
Chronic illness support
Wearable pain management technologies offer valuable support for people with chronic illnesses by:
- Providing continuous pain relief
- Reducing medication side effects
- Improving quality of life
The integration of these devices into chronic pain management strategies can lead to more personalized and effective treatment plans.
Researchers frequently use wearable devices in clinical trials to test their effectiveness.
Rehabilitation and physical therapy

Wearable pain management devices are increasingly integrated into rehabilitation programs, offering:
- Targeted pain relief during exercises
- Progress tracking
- Improved compliance (people following through with doctor instructions)
This integration can lead to more effective rehabilitation outcomes and faster recovery times.
A clinical trial in the Archives of Physical Medicine and Rehabilitation showed that TENS alone or combined with exercise or physical therapy, helped reduce knee pain and improve mobility. The combined therapy was particularly effective, showing a significant decrease in light-intensity activity time and potentially lowering psychological barriers to exercise. The results suggest this approach could be a valuable strategy for people struggling with knee pain and sedentary behavior.
Workplace ergonomics and injury prevention

Healthcare providers use wearable technologies in occupational health settings to:
- Prevent workplace injuries
- Manage chronic pain for employees
- Improve ergonomics (physical comfort)
A study in Advanced Intelligent Systems found that implementing wearable pain management devices in the workplace can alleviate work-related pain and injuries.
By providing real-time feedback and pain management, these devices can help create safer and more comfortable work environments.
How to Choose the Right Wearable Pain Management Solution
With numerous options available, you should carefully consider several factors to select the right wearable pain management device for you.
Considerations when selecting a device

When choosing a wearable pain management solution, make note of its:
- Functions that help relieve your type of pain condition
- Device features and functionality
- Ease of use and comfort
- Battery life and portability
- Clinical evidence supporting its effectiveness
It’s important to consult with your healthcare provider to determine which device is best suited for your specific needs and condition.
Cost and insurance considerations

The cost of wearable pain management devices can vary widely. Consider:
- Initial device cost
- Ongoing expenses
- Insurance coverage options
While these devices may have higher upfront costs, they could lead to long-term savings in pain-related healthcare expenses. Research published in Cureus showed that despite higher upfront costs, wearable pain management devices resulted in lower overall pain-related healthcare expenses for participants.
User experience and comfort
The effectiveness of a wearable pain management device often depends on whether you use it correctly and consistently, and your comfort. Look for devices that offer:
- Adjustable settings
- Lightweight and discreet design
- Easy-to-use controls
85% of the 90% of participants in a 2020 pilot study who used a device more than half of the study period reported high user satisfaction scores. This suggests that you’re more likely to use a device that’s comfortable and easy to use consistently, leading to better pain management outcomes.
Clinical validation and research

When selecting a wearable pain management device, prioritize those with strong clinical evidence that shows they’re effective. Look for:
- Peer-reviewed studies
- Clinical trial results
- Food and Drug Administration (FDA) approval (in the United States)
Personalization and adaptability
Choose a device tailored to your specific needs and pain patterns. Look for features such as:
- Customizable treatment programs
- Multiple pain relief modes
- Integration with pain-tracking apps
Future of Wearable Pain Management
The field of wearable pain management is rapidly evolving, with exciting developments on the horizon.
Emerging technologies

Future wearable pain management devices may incorporate:
- Nanotechnology for targeted drug delivery
- Advanced materials for improved comfort and effectiveness
- Virtual reality integration for pain distraction (scientists have found that VR is effective for significant pain)
- Home-based monitoring (also known as RPM or remote patient monitoring)
These emerging technologies could significantly improve pain management outcomes in the coming years.
A report in Frontiers in Bioengineering and Biotechnology predicts that these emerging technologies will improve pain management outcomes.

Artificial intelligence integration
AI plays an important role in wearable pain management, offering:
- More accurate pain prediction
- Personalized treatment optimization
- Real-time treatment adjustments
For example, an automated pain recognition system using AI holds promise as an unbiased method to detect pain before, during, and after surgery.
Personalized medicine approaches

The future of wearable pain management includes highly personalized solutions, such as:
- Genetic-based treatment recommendations
- Integration with other health data (sleep patterns, stress levels)
- Adaptive learning algorithms for continuous improvement
These personalized approaches could lead to significantly better health outcomes and more effective pain management strategies.

Potential for home-based pain management
Advancements in wearable technologies may lead to more comprehensive home-based pain management solutions, offering:
- Remote monitoring by healthcare providers
- Integration with smart home devices
- Improved long-term pain management strategies
This shift towards home-based care can reduce hospital visits and improve the overall quality of life for chronic pain patients.
Research in Pain Therapy suggests that home-based wearable pain management devices reduce hospital visits for chronic pain.
Interdisciplinary research developments
The future of wearable pain management will likely involve collaboration across various fields, including:
- Neuroscience
- Materials science
- Data analytics
- Behavioral psychology
This interdisciplinary approach could lead to breakthroughs in pain management, which could decrease how many people have chronic pain in the coming years.
Wearable pain management represents a promising frontier in healthcare technology. As devices become more sophisticated, personalized, and accessible, individuals suffering from chronic pain can look forward to more targeted, non-invasive relief strategies. The future of pain management is not just about treating symptoms, but understanding and addressing pain at its source.
References
AI pain recognition system could help detect patients’ pain before, during and after surgery. (2023). American Society of Anesthesiologists. Retrieved from https://www.asahq.org/about-asa/newsroom/news-releases/2023/10/ai-pain-recognition-system
Alberts, N.M., Leisenring, W., Flynn, J.S., Whitton, J., et al. (2020). Wearable Respiratory Monitoring and Feedback for Chronic Pain in Adult Survivors of Childhood Cancer: A Feasibility Randomized Controlled Trial From the Childhood Cancer Survivor Study. JCO Clinical Cancer Informatics, 4. doi.org/10.1200/CCI.20.00070
Andrade, R., Duarte, H., Pereira, R., Lopes, I., Pereira, H., Rocha, R., & Espregueira-Mendes, J. (2016). Pulsed electromagnetic field therapy effectiveness in low back pain: A systematic review of randomized controlled trials. Porto Biomedical Journal, 1(5), 156. doi.org/10.1016/j.pbj.2016.09.001
Bara, R. O., Lee, M., Phan, T., Pacheco, M., Camargo, A. F., Kazmi, S. M., Rouzi, M. D., Modi, D., Shaib, F., & Najafi, B. (2024). Transcutaneous electrical nerve stimulation for fibromyalgia-like syndrome in patients with Long-COVID: A pilot randomized clinical trial. Scientific Reports, 14(1), 1-11. doi.org/10.1038/s41598-024-78651-5
Beyond Traditional Healing: How AI Enhances Biofeedback for Pain Management. (2023). Retrieved from https://ospinamedical.com/orthopedic-blog/beyond-traditional-healing-how-ai-enhances-biofeedback-for-pain-management
Casarin, S., Haelterman, N. A., & Machol, K. (2024). Transforming personalized chronic pain management with artificial intelligence: A commentary on the current landscape and future directions. Experimental Neurology, 382, 114980. doi.org/10.1016/j.expneurol.2024.114980
Chen, J., Jin, T., & Zhang, H. (2020). Nanotechnology in Chronic Pain Relief. Frontiers in Bioengineering and Biotechnology, 8, 557957. doi.org/10.3389/fbioe.2020.00682
Chronic pain: Medication decisions. MayoClinic. Retrieved from https://www.mayoclinic.org/chronic-pain-medication-decisions/art-20360371
Cox, A. (2024). Insights into Emerging Technologies in Pain Medicine. Retrieved from https://www.managedhealthcareexecutive.com/view/insights-into-emerging-technologies-in-pain-medicine
Cudejko T, van der Esch M, van der Leeden M, van den Noort JC, Roorda LD, Lems W, Twisk J, Steultjens M, Woodburn J, Harlaar J, Dekker J. The immediate effect of a soft knee brace on pain, activity limitations, self-reported knee instability, and self-reported knee confidence in patients with knee osteoarthritis. (2017). Arthritis Research and Therapy;19(1):260. doi: 10.1186/s13075-017-1456-0
Deswal, P. (2024). NXTSTIM’s wearable nerve stimulation device helps manage long-term pain. Clinical Trials Arena. Retrieved from https://www.clinicaltrialsarena.com/news/nxtstims-wearable-nerve-stimulation-device-helps-manage-long-term-pain/
Different Types of Chronic Pain. (2020). Southern Pain and Neurological. Retrieved from https://southernpainclinic.com/blog/different-types-of-chronic-pain/
El-Tallawy, S.N., Pergolizzi, J.V., Vasiliu-Feltes, I., et al. (2024). Innovative Applications of Telemedicine and Other Digital Health Solutions in Pain Management: A Literature Review. Pain and Therapy, 13, 791–812. doi.org/10.1007/s40122-024-00620-7
Gagnon, M.P., Ouellet, S., Attisso, E., Supper, W., Amil, S., Rhéaume, C., Paquette, J.S., Chabot, C., Laferrière, M.C., Sasseville, M. (2024). Wearable Devices for Supporting Chronic Disease Self-Management: Scoping Review. Interactive Journal of Medical Research,3:e55925. doi: 10.2196/55925
How Wearable Devices Are Shaping the Future of Chronic Pain Management. Pain Mgmt Advancements. Retrieved from https://advancementsinpainmanagement.com/therapeutic-care/patient-monitoring/how-wearable-devices-shaping-chronic-pain-management/
Huhn, S., Axt, M., Gunga, C., Maggioni, M. A., Munga, S., Obor, D., Sié, A., Boudo, V., Bunker, A., Sauerborn, R., Bärnighausen, T., & Barteit, S. (2022). The Impact of Wearable Technologies in Health Research: Scoping Review. JMIR MHealth and UHealth, 10(1), e34384. https://doi.org/10.2196/34384
Johnson, M. I., & Jones, G. (2017). Transcutaneous electrical nerve stimulation: current status of evidence. Pain Management, 7(1), 1-4. Retrieved from Transcutaneous electrical nerve stimulation: current status of evidence
Koch, R. Researchers discover localised pain relief using known chemical reaction. (2024). University of Adelaide. Retrieved from https://www.adelaide.edu.au/newsroom/news/list/2024/11/04/researchers-discover-localised-pain-relief-using-known-chemical-reaction
Management of Chronic Pain. (2023). National Commission on Correctional Health Care (NCCHC). Retrieved from https://www.ncchc.org/position-statements/management-of-noncancer-chronic-pain-2023/
Non-Traditional Pain Management. (2023). ProCare Rx HospiceCare. Retrieved from https://www.procarehospicecare.com/non-traditional-pain-management
Nowosielski, B. Biofeedback Shows Promising Results in Treating Chronic Pain. (2025). Retrieved from https://www.drugtopics.com/view/biofeedback-shows-promising-results-in-treating-chronic-pain
Objective wearable measures correlate with self-reported chronic pain levels in people with spinal cord stimulation systems. (2023). npj Digital Medicine. Retrieved from https://www.nature.com/articles/s41746-023-00892-x
Patel, V., Chesmore, A., Legner, C. M., & Pandey, S. (2022). Trends in Workplace Wearable Technologies and Connected-Worker Solutions for Next-Generation Occupational Safety, Health, and Productivity. Advanced Intelligent Systems, 4(1), 2100099. doi.org/10.1002/aisy.202100099
Rebelo, A., Martinho, D.V., Valente-dos-Santos, J. et al. (2023). From data to action: a scoping review of wearable technologies and biomechanical assessments informing injury prevention strategies in sport. BMC Sports Science, Medicine and Rehabilitation, 15, 169 doi.org/10.1186/s13102-023-00783-4
Ross, E. L., Jamison, R. N., Nicholls, L., Perry, B. M., & Nolen, K. D. (2020). Clinical Integration of a Smartphone App for Patients With Chronic Pain: Retrospective Analysis of Predictors of Benefits and Patient Engagement Between Clinic Visits. Journal of Medical Internet Research, 22(4), e16939. doi.org/10.2196/16939
Sensors and Devices Guided by Artificial Intelligence for Personalized Pain Medicine. (2024). Cyborg and Bionic Systems. Retrieved from https://spj.science.org/doi/10.34133/cbsystems.0160
Smart patch combines real-time health monitoring and drug delivery. (2025). Medical Xpress. Retrieved from https://medicalxpress.com/news/2025-02-smart-patch-combines-real-health.html
Spiegel, B., Fuller, G., Lopez, M., Dupuy, T., Noah, B., Howard, A., Albert, M., Tashjian, V., Lam, R., Ahn, J., Dailey, F., Rosen, B. T., Vrahas, M., Little, M., Garlich, J., Dzubur, E., IsHak, W., & Danovitch, I. (2019). Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE, 14(8), e0219115. doi.org/10.1371/journal.pone.0219115
Tepper, S.J., McAllister, P., Monteith, T. (2024). Update on Noninvasive Neuromodulation for Headache Treatment. Practical Neurology (US).;23(4):23-28.
Trafton, A. Wearable patch can painlessly deliver drugs through the skin. (2023). Massachusetts Institute of Technology. Retrieved from https://news.mit.edu/2023/wearable-patch-can-painlessly-deliver-drugs-through-skin-0419
Transcutaneous Electrical Nerve Stimulation for Pain Control. (2024). Head & Neck Pain Clinic. Retrieved from https://mhnpc.com/2024/10/28/transcutaneous-electrical-nerve-stimulation-for-pain-control/
Weatherly, S., McKenna, T., Wahba, S., Friedman, A., Goltry, W., Wahid, T., Abourahma, H., Lee, K., Rehman, A., Odeh, A., & Costin, J. (2024). Effectiveness of Digital Health Interventions (DHI) in Chronic Pain Management: A Scoping Review of Current Evidence and Emerging Trends. Cureus, 16(10), e72562. doi.org/10.7759/cureus.72562
Why Traditional Pain Management Doesn’t Work for Many With Chronic Pain. Michigan Integrative Health. Retrieved from https://michiganih.com/why-traditional-pain-management-doesnt-work-for-many-with-chronic-pain/
Yamada, K., Shimizu, H., Doi, N., Harada, K., et al. (2025). Usefulness and Safety of a Wearable Transcutaneous Electrical Nerve Stimulation Device for Promoting Exercise Therapy in Patients With Chronic Knee Pain: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, 106 (2), 167-176. doi: 10.1016/j.apmr.2024.08.021
Zhu, Y., Yao, Y., Kuang, R., Chen, Z., Du, Z., & Qu, S. (2023). Global research trends of nanotechnology for pain management. Frontiers in Bioengineering and Biotechnology, 11, 1249667. https://doi.org/10.3389/fbioe.2023.1249667